Understanding Blood Clots and Autoimmune Diseases
When we think about blood clots and autoimmune diseases, it might not be immediately evident how these two health conditions are connected. Blood clots are a natural part of the body's response to injury and can help to prevent excessive bleeding. Autoimmune diseases, on the other hand, occur when the body's immune system mistakenly attacks healthy cells. In this article, we will delve into the link between blood clots and autoimmune diseases, exploring the various ways in which these two seemingly separate health issues can intersect.
The Role of Inflammation in Blood Clot Formation
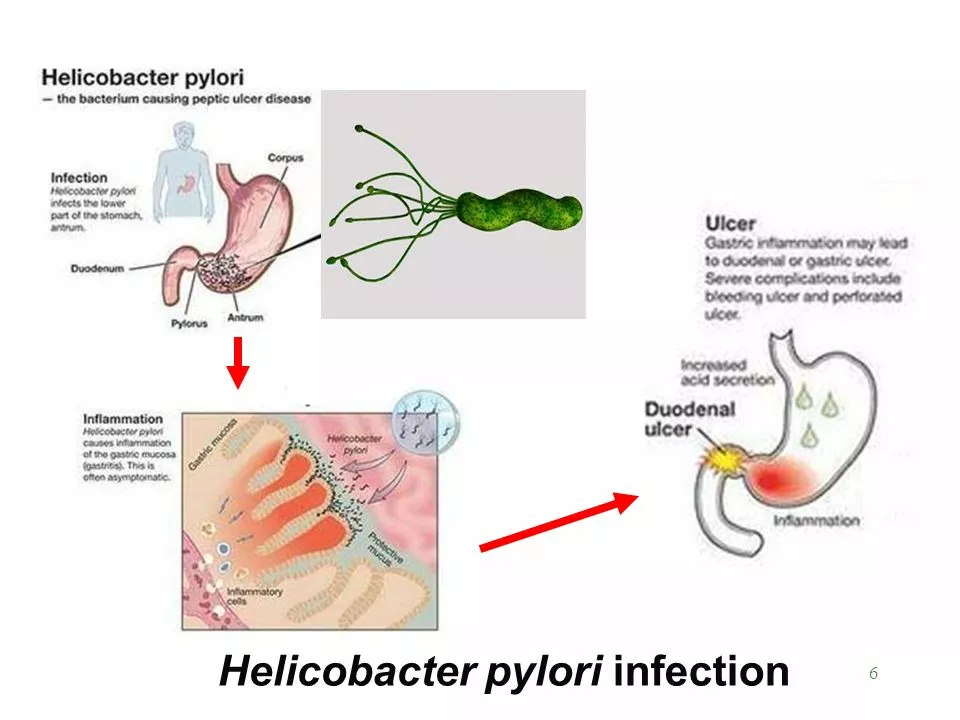
One of the key factors that connects blood clots to autoimmune diseases is inflammation. Inflammation is the body's natural response to injury or infection, and it plays a crucial role in the healing process. However, when inflammation becomes chronic or excessive, it can lead to the formation of blood clots. This is because inflammation can cause the blood vessels to constrict and the blood to become more prone to clotting, creating a potentially dangerous situation.
Autoimmune diseases often involve chronic inflammation, as the immune system is constantly attacking healthy cells and tissues. This ongoing inflammation can increase a person's risk of developing blood clots, particularly in individuals who have certain autoimmune diseases that target the blood vessels, such as lupus or vasculitis.
Antiphospholipid Syndrome: A Direct Link Between Autoimmunity and Blood Clots
Antiphospholipid Syndrome (APS) is an autoimmune disease that directly causes blood clot formation. People with APS have antibodies that target phospholipids, which are essential components of cell membranes. These antibodies can cause the blood to become more prone to clotting, leading to an increased risk of developing blood clots in the veins and arteries.
APS can occur on its own or in conjunction with other autoimmune diseases, such as lupus. In fact, up to 30% of individuals with lupus also have APS, making blood clot formation a significant concern for these patients. It is essential for individuals with APS or other autoimmune diseases to be aware of their increased risk of blood clots and to take appropriate measures to reduce this risk.
Managing the Risk of Blood Clots in Autoimmune Disease Patients
For individuals with autoimmune diseases, managing the risk of blood clot formation is a crucial aspect of their overall health care plan. This may involve several different strategies, including:
- Regular blood tests to monitor clotting factors and inflammation levels
- Using anticoagulant medications, such as warfarin, to prevent blood clots
- Managing inflammation through the use of anti-inflammatory medications or other treatments, such as corticosteroids or immunosuppressive drugs
- Lifestyle changes, such as maintaining a healthy weight, exercising regularly, and not smoking, to reduce the risk of blood clot formation
It is essential for individuals with autoimmune diseases to work closely with their healthcare providers to develop a personalized plan for managing their risk of blood clots. This may involve regular check-ups, ongoing monitoring, and adjustments to medications or treatment plans as needed.
Conclusion: Understanding the Connection and Taking Action
While blood clots and autoimmune diseases may seem like separate health issues, they are closely connected through the common factor of inflammation. Individuals with autoimmune diseases are at an increased risk of developing blood clots, particularly if they have APS or other conditions that directly target the blood vessels. By understanding this connection, patients and healthcare providers can work together to develop targeted strategies for managing the risk of blood clots and maintaining overall health in the context of autoimmune disease.



Diane Larson on 6 May 2023, AT 23:58 PM
First off, thanks for pulling together such a thorough overview of how inflammation bridges blood clots and autoimmune disorders. The way you broke down the pathophysiology makes it easier for newcomers to grasp why chronic inflammation isn’t just a symptom but a driver of thrombosis. Highlighting antiphospholipid syndrome as a concrete example really grounds the discussion in something patients can relate to. I also appreciate the clear checklist of management steps – from routine labs to lifestyle tweaks – because it gives readers actionable items right away. One point that could be expanded is how specific cytokines, like IL-6 and TNF-alpha, amplify the coagulation cascade; that connection is becoming a hot topic in research. It might be worth mentioning newer therapeutic options targeting those cytokines, especially for patients who can’t tolerate traditional immunosuppressants. Also, the role of endothelial dysfunction in vasculitis deserves a short paragraph, since it directly feeds into clot formation. Your section on anticoagulation could clarify the differences between warfarin and direct oral anticoagulants, because many patients ask which is safer in the context of lupus. A brief note on monitoring for bleeding complications would round that out nicely. The lifestyle advice is solid – maintaining a healthy weight, regular exercise, and smoking cessation are cornerstone strategies for everyone, not just those with autoimmunity. Perhaps you could add a tip about staying hydrated, especially during long flights, as dehydration is a known clot risk factor. Overall, the article strikes a good balance between scientific depth and readability. Keep up the great work, and thanks for shedding light on a topic that often flies under the radar.