Introduction to Genital Psoriasis and Calcipotriol
As someone who has struggled with genital psoriasis, I know firsthand how difficult it can be to find effective treatments for this sensitive area. Psoriasis is a chronic skin condition characterized by the rapid overgrowth of skin cells, leading to the formation of red, scaly patches. Genital psoriasis affects the skin in the genital area, often causing discomfort, itching, and irritation. Calcipotriol, a synthetic form of vitamin D, has been found to be a promising treatment option for genital psoriasis. In this article, we will explore the benefits of calcipotriol and other treatments for genital psoriasis, as well as important considerations for using these therapies.
Understanding the Causes and Symptoms of Genital Psoriasis
Before diving into treatment options, it's essential to understand what causes genital psoriasis and its symptoms. Like other forms of psoriasis, genital psoriasis is an autoimmune condition, meaning that the immune system mistakenly attacks healthy skin cells. This leads to an overproduction of skin cells, causing the characteristic red, scaly patches.
Symptoms of genital psoriasis can vary from person to person but typically include redness, itching, burning, and soreness in the genital area. The skin may also crack or bleed, and the condition can cause significant emotional distress due to its sensitive location. Understanding these causes and symptoms can help us better navigate treatment options and considerations for managing genital psoriasis.
Calcipotriol: An Overview of This Vitamin D Derivative
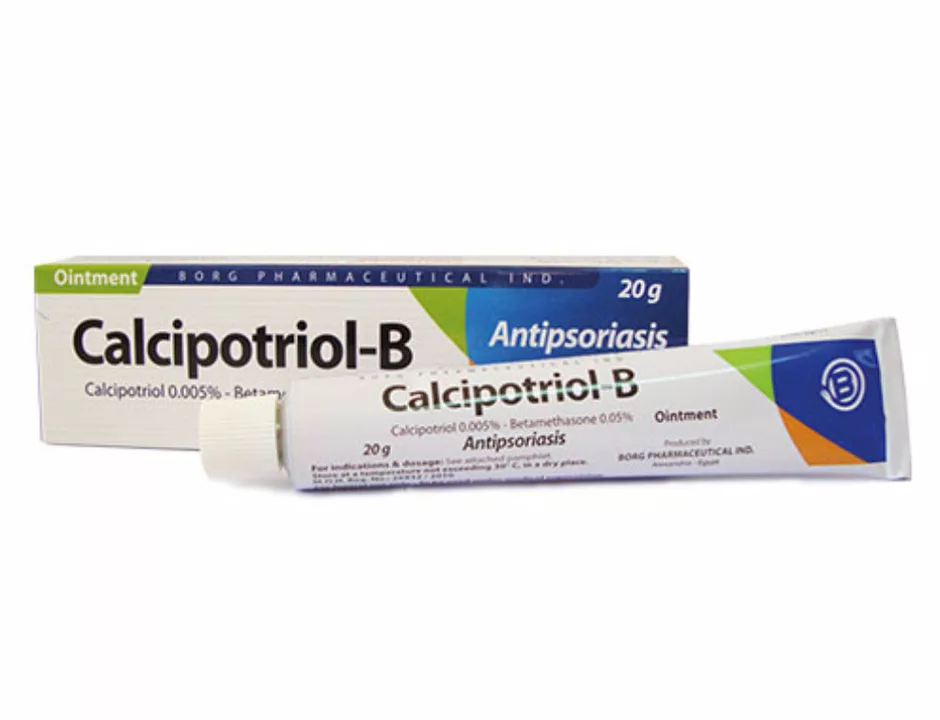
Calcipotriol is a synthetic form of vitamin D, which has been found to be an effective treatment for psoriasis. It works by slowing down the overproduction of skin cells, thereby reducing the symptoms of psoriasis. Calcipotriol is available as a cream, ointment, or scalp solution, and has been shown to be particularly effective in treating genital psoriasis due to its low potential for skin irritation.
It's important to note that calcipotriol is not a cure for psoriasis, but it can help manage symptoms and improve the appearance of the skin. Additionally, it's essential to follow your healthcare provider's instructions for proper use and dosage of calcipotriol, as misuse can lead to side effects.
Topical Corticosteroids: A Common Treatment for Genital Psoriasis
Topical corticosteroids are another common treatment for genital psoriasis. These medications work by reducing inflammation and suppressing the immune system's overactive response, which helps to decrease symptoms. Topical corticosteroids come in various strengths, but it's crucial to use low-potency corticosteroids in the genital area due to the increased risk of side effects.
While topical corticosteroids can be highly effective in treating genital psoriasis, they should be used sparingly and only as directed by your healthcare provider. Long-term use of corticosteroids can lead to thinning of the skin and other side effects.
The Role of Moisturizers in Genital Psoriasis Management
Moisturizers play a vital role in the management of genital psoriasis, as they help to soothe irritated skin and prevent cracking and bleeding. It's essential to choose a fragrance-free, hypoallergenic moisturizer to minimize the risk of further irritation. It's also important to apply the moisturizer regularly, especially after bathing, as this can help to lock in moisture and promote healing.
While moisturizers alone may not be sufficient to treat genital psoriasis, they can be an essential part of your overall treatment plan when used in conjunction with other therapies, such as calcipotriol or topical corticosteroids.
Phototherapy: A Light-Based Treatment for Psoriasis
Phototherapy, or light therapy, is another treatment option for psoriasis, including genital psoriasis. This therapy involves exposing the skin to ultraviolet (UV) light, which can help to slow down the overproduction of skin cells and reduce inflammation. Phototherapy can be administered in a healthcare provider's office, or at home with a prescribed UV light device.
While phototherapy can be effective in treating psoriasis, it's important to discuss the potential risks and benefits with your healthcare provider, as UV light can also increase the risk of skin cancer and other side effects.
Systemic Medications for Severe Genital Psoriasis
In some cases, genital psoriasis may be severe or unresponsive to topical treatments, necessitating the use of systemic medications. These medications, which include oral drugs and injections, work by suppressing the immune system and reducing inflammation throughout the body. Some examples of systemic medications for psoriasis include methotrexate, cyclosporine, and biologic drugs like adalimumab and etanercept.
While systemic medications can be highly effective in treating severe genital psoriasis, they also come with a risk of significant side effects and should be reserved for cases where other treatments have failed or are contraindicated.
Lifestyle Considerations for Managing Genital Psoriasis
Managing genital psoriasis involves more than just medical treatments—it also requires attention to lifestyle factors that can impact the severity of symptoms. Some lifestyle considerations for managing genital psoriasis include maintaining good hygiene, avoiding harsh soaps and chemicals that can irritate the skin, wearing loose-fitting, breathable clothing, and managing stress levels, as stress can exacerbate psoriasis symptoms.
By paying attention to these lifestyle factors, you can help to create an environment that promotes healing and minimizes the risk of psoriasis flare-ups in the genital area.
Working With Your Healthcare Provider to Develop a Treatment Plan
When it comes to treating genital psoriasis, it's crucial to work closely with your healthcare provider to develop a treatment plan that addresses your unique needs and symptoms. This may include a combination of treatments, such as calcipotriol, topical corticosteroids, moisturizers, and lifestyle modifications.
By maintaining open communication with your healthcare provider and following their recommendations for treatment, you can increase your chances of successfully managing your genital psoriasis and improving your quality of life.


Samantha Vondrum on 27 April 2023, AT 05:57 AM
Dear readers, I commend you for seeking reliable information on a sensitive condition such as genital psoriasis. Calcipotriol, being a vitamin D analogue, offers a gentle yet effective approach for many patients. It is essential to pair this therapy with a fragrance‑free moisturizer to maintain skin barrier integrity 😊. Always consult your dermatologist to tailor the regimen to your specific needs and to monitor for any adverse effects. Together, we can navigate this journey with compassion and scientific rigor.