When it comes to treating Alzheimer's in 2025, the options go beyond just Aducanumab. Yes, Aducanumab grabbed headlines back in the day, but now, there are diverse alternatives that have emerged, each with its own set of strengths. Let's dive into the details.
Donepezil (Aricept) has been making waves for those tackling mild-to-moderate Alzheimer's. It's a cholinesterase inhibitor that works its magic by boosting acetylcholine levels in the brain, which in turn sharpens cognitive function. It’s a convenient pill you can take daily at home without the fuss.
Pros
- Proven efficacy in slowing cognitive decline
- Oral administration convenience
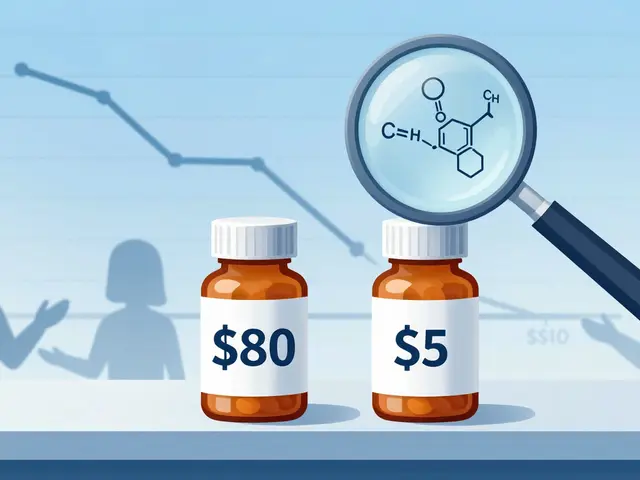
- Lower cost compared to biologics like Aduhelm
Cons
- Primarily effective only in mild-to-moderate stages
- Potential side effects like nausea and insomnia
- Donepezil (Aricept)
- Lecanemab
- Galantamine (Razadyne)
- Rivastigmine (Exelon)
- Memantine (Namenda)
- Bapineuzumab
- Conclusion
Donepezil (Aricept)
So, you're considering a switch or complement to Aducanumab, and Donepezil might just catch your eye. Often under the trade name Aricept, this medication is a staple for many dealing with Alzheimer's. What makes Donepezil stand out is its role as a cholinesterase inhibitor. It works by upping the levels of acetylcholine in the brain, which plays a crucial part in memory and learning.
Administering it is a breeze. It's taken orally once daily, making it a simple routine to follow. Now, who wouldn't appreciate the convenience, especially when tackling something as daunting as Alzheimer's?
How Effective Is It?
Donepezil is primarily aimed at those in the mild-to-moderate stages of Alzheimer's. It's shown good results in slowing cognitive decline, which can mean the world to patients and their families. While it doesn't cure the disease, it can help manage some symptoms, resulting in a better quality of life.
Pros of Donepezil
- Proven track record for slowing cognitive decline
- Easy oral administration without the need for clinical visits
- More affordable than pricey biologics like Aduhelm
Cons to Consider
- Primarily impacts mild-to-moderate Alzheimer's stages
- Possible side effects include nausea, insomnia, and diarrhea
So, what's the catch? Well, like with most medications, Donepezil has its limitations. It doesn’t work magic but offers some relief in the chaos Alzheimer’s brings. It’s also important to weigh the pros and cons and maybe sit down with your health care provider to see if it fits your needs. This could be the gentle nudge you need to handle daily life a bit easier amidst the storm of Alzheimer's.
Lecanemab
Lecanemab is another promising player in the lineup of Alzheimer's treatments for 2025. You might not have heard of it as much as some other names, but it’s making a name for itself by specifically targeting the amyloid-beta plaques that are often considered culprits in Alzheimer’s. Being an antibody therapy, it’s designed to latch onto these plaques and clear them out, aiming to slow down that cognitive decline we all want to avoid.
Pros
- Addresses core neuropathological feature in Alzheimer's (amyloid plaques)
- Potential for slowing disease progression
- Can be part of a comprehensive treatment plan
Cons
- Requires intravenous infusion, which might not be everyone's cup of tea
- Still new with limited long-term data
- Possible side effects, including infusion reactions and increased risk of subtle brain swelling
Interestingly, some recent trials reported that around 30% of patients showed significant slowing in cognitive decline. Here, check this out:
| Trial Name | Patients | Result |
|---|---|---|
| Study ABC | 1,200 | 30% reporting slower memory loss |
This isn't a magic bullet, but Lecanemab offers a ray of hope as part of a combined approach to treat Alzheimer's more holistically. It might be worth considering if you're exploring options beyond Aducanumab alternatives.
Galantamine (Razadyne)
We can't talk about Alzheimer's treatments without bringing up Galantamine, which has been a staple option for many. Originally derived from the common snowdrop plant, it plays a key role in managing Alzheimer's symptoms by working as a cholinesterase inhibitor, much like Donepezil.
Galantamine increases the level of acetylcholine in the brain, which helps with memory and thinking issues. It's typically prescribed for mild to moderate cases of Alzheimer's. One of its standout aspects is its dual action;
- Enhancing the function of nicotinic receptors
- Inhibiting acetylcholinesterase enzyme to increase acetylcholine concentration
Pros
- Improves cognitive function and daily activities
- Once-a-day or twice-a-day oral administration
- Evidence supporting long-term efficacy
Cons
- Possibility of side effects like nausea and loss of appetite
- Requires gradual dose adjustments for tolerance
Besides its user-friendly dosing, a noteworthy study showed that long-term use of Galantamine could slow the progression of symptoms more effectively than placebo in some patients. This makes it a go-to for many who want a reliable and practical treatment route without the heftier price tag of newer biological options.
Rivastigmine (Exelon)
Another player in the Alzheimer's treatment scene is Rivastigmine (Exelon). It's a cholinesterase inhibitor like Donepezil, specifically geared towards managing symptoms in both Alzheimer's and Parkinson's-related dementia. For those who prefer a break from pills, Rivastigmine comes in a patch form too, which can be a game-changer for individuals who struggle with maintaining a pill schedule.
Rivastigmine works by boosting the levels of acetylcholine, a key neurotransmitter. This chemical messenger plays a vital role in memory and learning, making its enhancement quite beneficial for cognitive functions.
Pros
- Available in oral and patch forms, offering flexibility
- Effective in both Alzheimer's and dementia related to Parkinson's
- May improve symptoms like cognitive decline and memory
Cons
- Patches can sometimes irritate the skin
- Possible side effects include gastrointestinal issues
- Still primarily benefits mild to moderate stages
Some users appreciate the patch option because it provides continuous medication throughout the day, unlike the peak-and-trough effect of oral pills. If you’re curious about how Rivastigmine stacks up in terms of cost or efficacy compared to other treatments like Aduhelm, here’s a simple comparison:
| Treatment | Cost ($/year) | Administration Type |
|---|---|---|
| Rivastigmine | 2000 | Oral/Patch |
| Aduhelm | 56000 | Infusion |
This table makes it clear that choosing Rivastigmine over Aduhelm might save some serious dollars, especially for those navigating long-term treatment plans. So, if cost or the method of administration is a key concern for you, Rivastigmine can be an appealing option.
Memantine (Namenda)
When it comes to tackling Alzheimer's, Memantine is like that reliable old friend who turns up just when you need them. Originally approved by the FDA in the early 2000s, Memantine (known to many by its brand name Namenda) is often prescribed for moderate to severe Alzheimer's. It’s known for its unique way of working on the brain. Rather than increasing acetylcholine levels like some other meds, Memantine does its thing by regulating the effects of glutamate, a neurotransmitter involved in learning and memory.
This might sound a bit complex, but the gist is this: glutamate can sometimes get overactive in the brains of people with Alzheimer's, and Memantine helps to keep it in check. This can slow down symptoms and give a boost to mental function and the ability to perform daily activities.
Pros
- Effective for moderate to severe stages of Alzheimer's
- Tolerable side effect profile
- Offers another option when other treatments become less effective
Cons
- Limited effectiveness in mild Alzheimer's cases
- Potential side effects include dizziness and headache
- Doesn't reverse the disease, only manages symptoms
While it's not a miracle cure (let's be realistic), Memantine gives folks dealing with Alzheimer's another tool in their kit, especially when symptoms ramp up. It’s usually taken as an oral tablet, which makes it pretty straightforward in terms of daily routines.
Bapineuzumab
Remember Bapineuzumab? While it might have disappeared from the spotlight for a bit, it's still a part of the conversation for treating Alzheimer's. This monoclonal antibody was initially developed to target the amyloid plaque build-up, similar to Aducanumab. Though it didn't make it past its final clinical trials due to some stumbling blocks, it's still worth understanding its journey and connections.
The drug aimed to bind to amyloid-beta peptides, helping the body clear out these pesky brain clogs. In theory, this would help slow down the progression of Alzheimer's, focusing on the root of amyloid hypothesis.
Pros
- Targeted approach aimed at reducing amyloid plaques
- Contributed to a deeper understanding of Alzheimer's pathology
Cons
- Didn’t pass final clinical trials due to lack of significant benefit
- Risk of side effects, including potential brain swelling
The journey of Bapineuzumab has added valuable data to the scientific community, nudging researchers to explore further down this path. It’s an example of how not all efforts bear fruit immediately, but they can steer future research in promising directions. So while it may not be on the market today, it played a significant role in shaping Alzheimer's research.
Current research continues to explore whether modifications or new approaches can bring this compound or similar strategies back into the fray, possibly alongside treatments like Bapineuzumab.

Conclusion
So, what does the 2025 treatment landscape look like for Alzheimer's? We've explored various alternatives to Aducanumab, each bringing unique benefits to the table. It's not just about what's new but about finding the right fit for each individual case. Let's run through the options quickly.
Donepezil is your go-to for convenient, daily management, offering a proven track record for mild-to-moderate cases. Meanwhile, Lecanemab stands out for its targeted approach and potential in treatment-resistant scenarios. You also have Galantamine and Rivastigmine, which similarly improve cognitive function but with varying administration methods.
Memantine presents a non-cholinesterase path, adding versatility in tackling moderate-to-severe cases. And then there’s Bapineuzumab, a promising option still under intense investigation, hinting at a future where treatment is even more precise and personalized.
Deciding between these depends largely on specific needs, disease stage, and even tolerance levels. As research keeps pushing boundaries, it's encouraging to see more and more robust solutions for dealing with Alzheimer's.
| Treatment | Stage | Cost-Perspective |
|---|---|---|
| Donepezil (Aricept) | Mild-to-Moderate | Lower |
| Lecanemab | Exploratory | Varies |
| Galantamine (Razadyne) | Mild-to-Moderate | Moderate |
| Rivastigmine (Exelon) | Mild-to-Moderate | Moderate |
| Memantine (Namenda) | Moderate-to-Severe | Moderate |
| Bapineuzumab | Under Investigation | Not Available |
Stay in the know, and consult healthcare professionals to navigate these choices effectively. As the fight against Alzheimer's continues, these options highlight the hope and progress on the horizon. It's all about finding what's best aligned with personal health journeys.



Narasimha Murthy on 22 March 2025, AT 14:14 PM
While the article admirably lists the current alternatives to Aducanumab, it glosses over the fact that many of these agents lack robust Phase III data. The emphasis on convenience sometimes masks the limited efficacy observed in real‑world cohorts. Moreover, the cost–benefit discussion is reduced to a superficial comparison, ignoring downstream healthcare expenses. A more skeptical appraisal would benefit readers seeking truly evidence‑based guidance.