Getting Imipramine Timing and Dose Separation Right
When someone hands you that imipramine prescription, a hundred questions start popping up. When should I take it? What happens if I miss a dose? Will it mess up my other meds or my morning coffee? The timing with imipramine—an older tricyclic antidepressant—actually matters a lot more than with some newer meds.
If you’re curious, imipramine tends to have a pretty long half-life (about 11–25 hours), but it’s not the kind of drug you want to take here and there whenever you remember. Most doctors recommend taking it at the same time each day, and, in my house, that usually means after feeding my cat Alfie (who never lets me forget) and my dog Olive (who only cares if I drop some food). Make it part of your routine—whether it’s brushing your teeth or watching late-night reruns—to help keep blood levels steady.
Dose separation gets tricky if you’re on more than just imipramine. Some people need to space it from other medications, especially those that cause drowsiness or affect heart rhythm. If you ever feel dizzy or notice your heart beating funny, don’t brush it off—these meds can sometimes interact in sneaky ways. Mixing imipramine with anticholinergics (medications for allergies or overactive bladder) or antihistamines can crank up side effects, like dry mouth or constipation, so spacing doses by at least a couple of hours can help.
Got to take a sleeping pill or painkiller? Try to keep at least a few hours between imipramine and anything else sedating—otherwise, you could wake up foggy, cranky, or just not yourself. If you ever have to take antibiotics, especially some like erythromycin, double-check with your doctor or pharmacist. Same goes for mixing imipramine with certain heart or blood pressure meds.
Here’s an easy tip: jot down every medication you take—including over-the-counter and supplements—and bring the list to every appointment. Most drugstores offer printouts or apps that can help you keep it straight. And, if you’re the forgetful type or tend to doze off before taking meds at night, set a recurring reminder on your phone.
If you miss a dose, don’t double up the next time. That’s one shortcut you don’t want to take. Imipramine isn’t the kind of thing you want to flood your system with all at once. Just take your next dose at the regular time and move on.
And, yes, timing does make a difference with food. Taking imipramine with a light snack can soften the blow if you’re one of the unlucky few who get stomach upset. But for many, it’s fine on an empty stomach.
Just remember, the big stuff—the dangerous interactions—often sneak up when you add a new prescription and forget to mention your old ones. Don’t assume your doctor remembers everything; play it safe and mention imipramine every time you see a new provider.

Imipramine Interactions: Avoid Surprises
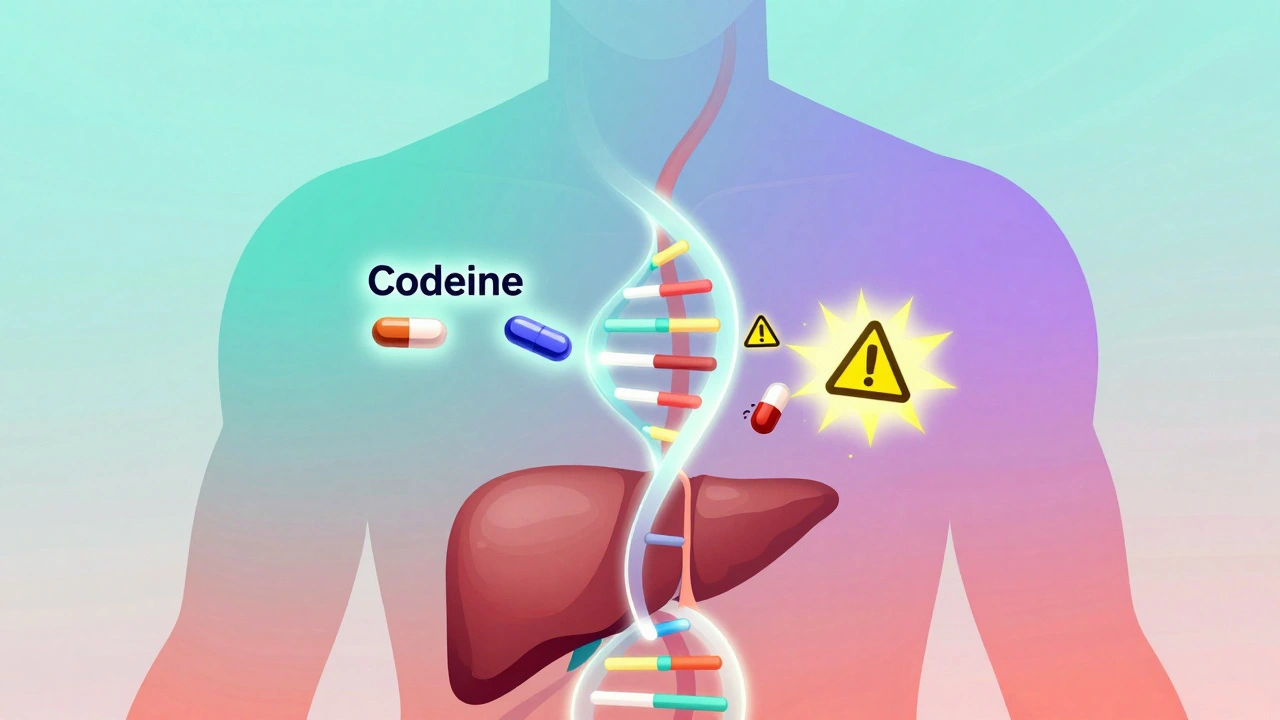
Imipramine is famous in medical circles for its potential to mix, match, and, sometimes, clash with lots of common meds. For starters, it shares a metabolic pathway in the liver (CYP2D6, for the curious), and plenty of other drugs—like certain SSRIs, antihistamines, and even some antipsychotics—use the same route. Too much competition and your imipramine levels can spike, which isn’t what you want.
Let’s break down some of the best-known interactions in plain English:
- SSRIs (like fluoxetine or paroxetine): These can raise imipramine levels, possibly leading to confusion, tremors, or irregular heartbeat.
- Anticholinergic drugs (found in allergy pills, some bladder meds): Take too many of these together, and you’ll get desert-like dry mouth, constipation, and blurred vision. Space them out by a few hours if you have to take both.
- MAO inhibitors: Never combine these with imipramine—you risk severe (sometimes fatal) high blood pressure, fever, or seizures.
- Alcohol and sedatives: Imipramine, as a tricyclic, already causes drowsiness in plenty of folks. Layer alcohol or a sleeping aid on top, and you might oversleep or wake up groggy (or not at all, which is much riskier).
- Heart medications: Some antiarrhythmics and blood pressure pills can interact with imipramine, increasing the risk of irregular heartbeat.
- St. John’s Wort and herbal supplements: Don’t assume natural is always safe. These can either boost or reduce imipramine’s effects unexpectedly.
Ever mixed meds and felt “off”? Don’t just ignore it. Reactions like sudden confusion, trouble urinating, shaking hands, or an oddly pounding heart are major red flags. If you Google interactions, don’t just stop at the first result. Reliable, detailed info is out there, and I always point people toward resources like this imipramine interaction FAQ. You’ll find drug names, real examples, and even instructions on what to do next if you’re worried.
Here’s another curveball: some cold medicines and even antacids (especially those with high sodium content) can affect how your body handles imipramine. Sounds wild, but that’s why doctors keep warning about “over-the-counter” dangers.
If you live with pets like Alfie and Olive, you know how much running around they need—same goes for tracking your meds. Always tell your doctor about every prescription, supplement, or even tea you’re taking. Doctors don’t mind hearing it again; trust me, they prefer you overshare than miss something important.
Sometimes people develop symptoms so slowly, they don’t connect it to their meds. You might get headaches, blurry vision, or feel oddly anxious or sluggish weeks after combining new treatments. It’s worth checking a recent med interaction table, like this one below, to spot patterns.
| Medication | Interaction Severity | Potential Effect |
|---|---|---|
| Fluoxetine | High | Increased side effects, confusion, heart rhythm changes |
| Diazepam | Moderate | Excess sedation, poor coordination |
| Diphenhydramine | Moderate | Extreme drowsiness, dry mouth, constipation |
| Metoprolol | Low | Possible blood pressure/bpm fluctuations |
Double-check with your pharmacist each time you pick up a refill, especially if your list of meds is growing. Don’t keep any secrets about new vitamins, herbs, or energy drinks just because they seem harmless—mixing some supplements with imipramine can really shake things up.

Smart Monitoring: Signs, Symptoms, and Lab Checks
You don’t need to turn into a hypochondriac, but you do need to know what to watch for with imipramine. First thing—side effects. This isn’t a mild-mannered antidepressant; it’s an old-school “tricyclic,” and folks can get everything from constipation and dizziness to dry mouth and blurry vision. It’s not rare to feel a little sleepy at first; your body usually adjusts after a week or two, but if the world still feels foggy, tell your doctor.
The serious stuff is all about your heart. Imipramine, especially in higher doses or combined with other meds, can change your heartbeat. You might feel palpitations, fluttering, tightness in your chest, or get faint in the shower (Olive has barked me back to consciousness more than once). If you have a personal or family history of heart issues, your provider might run an EKG before you start, then check again every few months.
A major fact many people miss: imipramine can cause your body to retain urine, raise your blood pressure, and—rarely—trigger seizures, especially if levels get too high. Anyone with kidney or liver problems needs close attention, sometimes with more frequent bloodwork.
Your doctor may order blood tests to check imipramine levels. This isn’t just busywork—it helps ensure you’re staying in that safe sweet spot. If you notice changes—a sudden headache, chest pain, blurred vision, or difficulty peeing—call your clinic. Those signals are warnings, not annoyances.
Some tips I tell everyone taking imipramine or mixing it with other meds:
- Track mood changes and side effects with a daily journal, even if it’s just voice notes after feeding the pets.
- Never stop imipramine “cold turkey.” Stopping all at once can leave you jittery, nauseous, and sometimes depressed or anxious. Taper down slowly with supervision.
- If you get constipated, up your fiber and fluids. It’s a small thing, but makes life much easier (and much less grumpy!).
- Stay hydrated. Dry mouth comes with the territory, but sipping water and chewing sugar-free gum actually help.
- Tell every new provider or dentist you see about your imipramine—even for something that seems unrelated, like a strange rash or tooth extraction.
- If you’re hospitalized, double-check that everyone knows you’re on it; this can affect anesthesia and pain medication.
With medication monitoring, you want to catch changes early. Most people see their prescribers every three to six months once things are steady, but if you feel weird or have new symptoms, don’t wait. You don’t get points for toughing it out.
Kids and teens need extra watching. Imipramine can sometimes spark mood swings or even increase suicidal thoughts in younger people. Families should keep the prescribing doc in the loop about any real changes in attitude, social life, or grades.
People sometimes hide side effects because they think they’re minor or expect to “get used to it.” Don’t. There are ways to tweak routines and dosages. Busy schedules, pet drama, or late-night pizza shouldn’t keep you from getting help when your body feels off.
If you need to dig into the science—or want to be the expert at your next doctor’s appointment—the imipramine interaction FAQ lays everything out, straight from the experts.
At the end of the day, taking imipramine (with or without additional meds) means paying attention and asking questions, not just going through the motions. Trust your own gut—if something doesn’t feel right, don’t just hope it’ll pass. And if you have pets, take a lesson from Alfie and Olive: making noise when you need something is the best way to get the help you deserve.




Selina M on 28 April 2025, AT 05:53 AM
Hey! imipramine can be a bit tricky but setting a daily reminder helps a lot
I like to pair it with my morning coffee so I never forget
Just make sure you dont take it right after a big meal if it upsets your stomach
And keep a note of any new meds you add