Understanding Myasthenia Gravis and Its Impact on Sleep
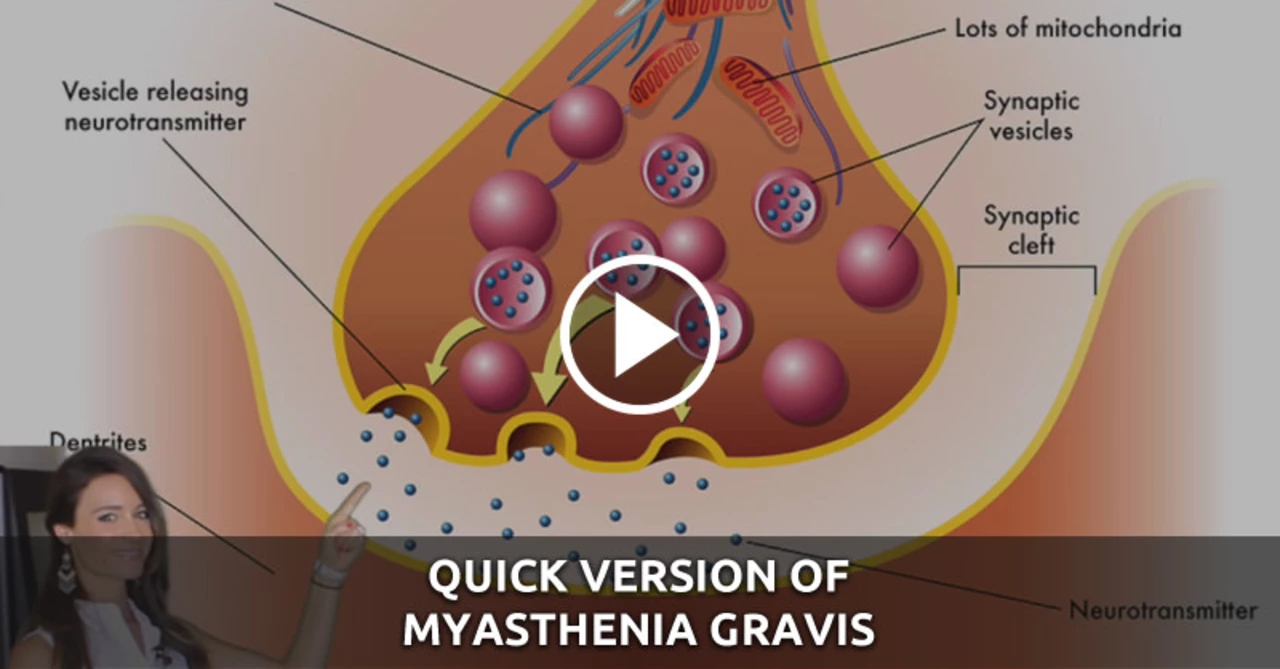
Myasthenia Gravis is an autoimmune neuromuscular disorder that affects the communication between nerves and muscles. This can lead to muscle weakness and fatigue, which can impact various aspects of life, including sleep.
As someone living with Myasthenia Gravis, I have experienced firsthand the challenges of getting a good night's sleep. In this article, I will share some tips and insights that have helped me and others with Myasthenia Gravis enjoy a more restful night's sleep.
Creating a Comfortable Sleep Environment
One of the first steps to ensuring a good night's sleep is creating a comfortable sleep environment. This can be especially important for those of us with Myasthenia Gravis, as muscle weakness and fatigue can make it difficult to get comfortable.
Start by choosing a supportive mattress and pillow that help maintain proper spinal alignment. Consider using a wedge pillow to elevate your head, which can help with breathing and reduce the risk of aspiration. Additionally, keep the room at a cool and comfortable temperature, and make sure it's dark and quiet.
Finally, avoid using electronic devices, such as smartphones and tablets, at least an hour before bedtime. The blue light emitted by these devices can interfere with the production of melatonin, a hormone that helps regulate sleep.
Establishing a Consistent Sleep Routine
Having a consistent sleep routine can greatly improve the quality of your sleep. This is particularly important for those with Myasthenia Gravis, as our bodies need time to recover from the day's activities.
Try to go to bed and wake up at the same time every day, even on weekends. This helps regulate your body's internal clock and can make it easier to fall asleep at night. Additionally, create a relaxing bedtime routine that signals to your body that it's time to wind down. This can include activities such as reading, listening to calming music, or taking a warm bath.
Avoid stimulating activities, such as exercise or engaging in intense conversations, close to bedtime. These can make it more difficult to fall asleep and may contribute to nighttime muscle fatigue.
Managing Symptoms and Medications
For those of us with Myasthenia Gravis, managing our symptoms and medications is crucial to achieving a restful night's sleep. Be sure to take your medications as prescribed and discuss any sleep-related side effects with your healthcare provider.
Some medications, such as corticosteroids, can cause insomnia or make it difficult to fall asleep. If this is the case, talk to your doctor about adjusting the timing of your medication doses or exploring alternative treatment options. Additionally, consider using over-the-counter sleep aids or natural supplements, such as melatonin or valerian root, to help improve your sleep. However, always consult your doctor before adding any new supplements to your regimen.
Finally, be proactive in managing your Myasthenia Gravis symptoms. Regular exercise, a healthy diet, and stress management techniques can all help reduce muscle weakness and fatigue, making it easier to sleep at night.
Adapting Sleep Positions for Better Breathing
For those of us with Myasthenia Gravis, finding a comfortable sleep position that allows for easy breathing can be a challenge. Muscle weakness can affect the muscles responsible for breathing, making it difficult to maintain a clear airway during sleep.
To help improve your breathing while sleeping, try sleeping on your side with a pillow between your knees. This position can help keep your airway open and reduce the risk of aspiration. Alternatively, consider using an adjustable bed or a wedge pillow to elevate your head and upper body. This can help with breathing and may also reduce symptoms of acid reflux, which can be common in people with Myasthenia Gravis.
If you continue to experience difficulty breathing while sleeping, consult your healthcare provider. They may recommend additional treatments or interventions, such as continuous positive airway pressure (CPAP) therapy, to help maintain an open airway during sleep.
Seeking Support and Adjusting Expectations
Living with Myasthenia Gravis can be challenging, and it's important to seek support from friends, family, and healthcare providers. Share your experiences and concerns with them, as they may be able to offer advice, encouragement, or simply a listening ear.
Additionally, consider joining a support group or online forum specifically for individuals with Myasthenia Gravis. Connecting with others who understand what you're going through can provide valuable insights and a sense of camaraderie.
Finally, adjust your expectations and be patient with yourself. Achieving a restful night's sleep with Myasthenia Gravis may take time and experimentation. Remember that everyone's experience with this condition is different, and what works for one person may not work for another. Stay open to trying new strategies and don't be afraid to reach out for help.



Javier Muniz on 12 May 2023, AT 23:36 PM
Hey folks, I've found that setting a consistent bedtime and keeping the room dark really helps my muscles relax enough to drift off. A supportive pillow and a cool temperature can make the difference between tossing and actually sleeping.