Understanding Amiloride and Its Mechanism of Action
Amiloride is a medication that is often prescribed for conditions such as heart failure and high blood pressure. But what exactly is it and how does it work? Let's delve into this medication to get a clearer understanding of its mechanism of action.
Amiloride is known as a potassium-sparing diuretic. This means that it helps your kidneys to get rid of excess sodium and water in the body, while also reducing the amount of potassium lost. This balance of electrolytes is crucial in maintaining a healthy heart and blood pressure levels.
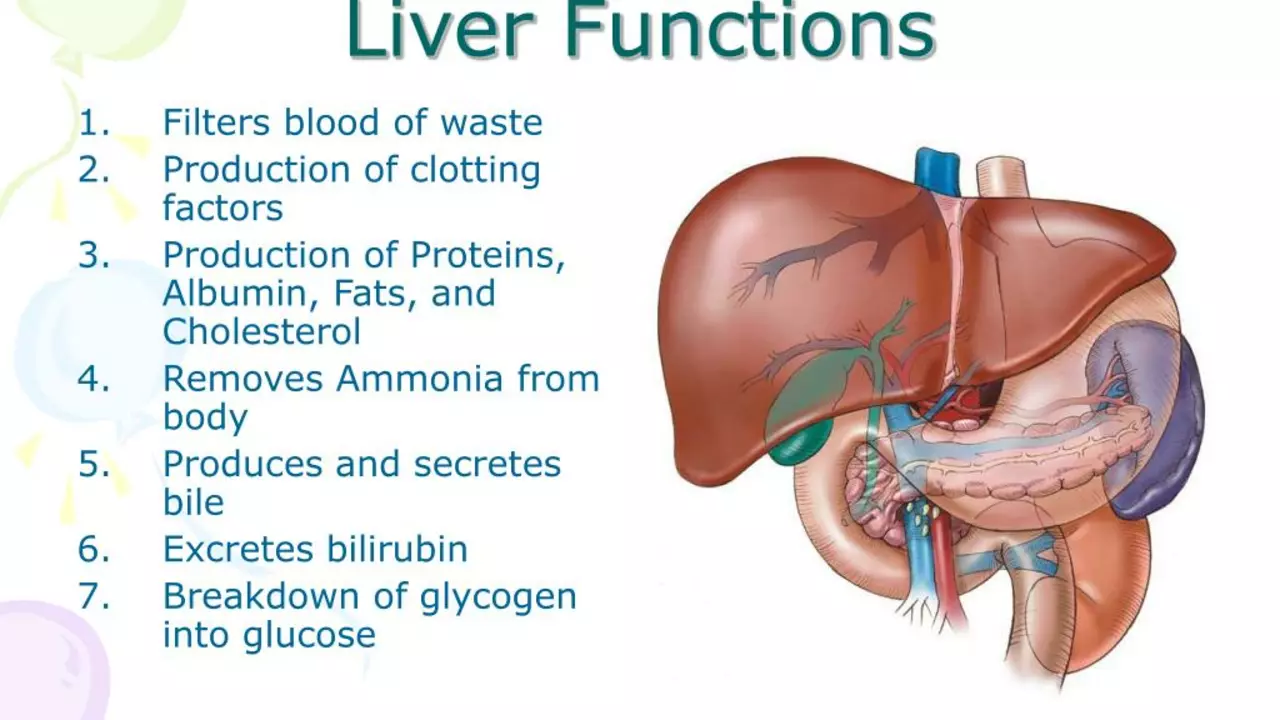
The Role of the Liver in Drug Metabolism
The liver plays a crucial role in the metabolism of drugs, including amiloride. It is responsible for the breakdown and elimination of drugs from the body. The process of drug metabolism can be broadly divided into two phases: Phase I and Phase II.
In Phase I, the liver uses enzymes to convert drugs into a form that can be easily excreted from the body. In Phase II, the liver further processes these substances, making them water-soluble so they can be easily removed by the kidneys.
What is Hepatic Impairment?
Hepatic impairment, or liver disease, is a broad term that covers all the potential problems that can cause the liver to function less efficiently. It can range from mild liver damage to severe liver failure. The liver is one of the most important organs in our body, responsible for hundreds of vital functions.
When the liver is impaired, it can no longer perform these functions effectively. This can result in a variety of symptoms, including jaundice, fatigue, and weight loss. The severity of liver disease can vary widely, from mild impairment to severe, life-threatening conditions.
Amiloride and Liver Function
Given the crucial role the liver plays in drug metabolism, it's clear to see why any impairment of liver function can impact how the body processes amiloride. If the liver is not functioning optimally, it may not be able to metabolize amiloride as effectively, leading to an increased risk of side effects.
In cases of severe hepatic impairment, there may be a need for dosage adjustments or even discontinuation of the drug. This is why it's so important for healthcare providers to monitor liver function in patients taking amiloride, particularly those with known liver disease.
Studies on the Impact of Amiloride on Liver Function
Several studies have been conducted to investigate the impact of amiloride on liver function. While more research is needed, the existing data provides some valuable insights. In general, these studies indicate that amiloride can be used safely in patients with hepatic impairment, as long as their liver function is closely monitored.
However, in cases of severe liver impairment, amiloride may need to be used with caution. These studies emphasize the need for regular liver function tests in patients taking this medication, particularly those with pre-existing liver disease.
Managing Amiloride Therapy in Patients with Liver Disease
Managing amiloride therapy in patients with liver disease can be a delicate balancing act. On one hand, amiloride can be a valuable treatment option for conditions like heart failure, which are often seen in patients with liver disease. On the other hand, the impaired liver function can affect how the body metabolizes the drug.
Regular monitoring of liver function is therefore key in these patients. This allows healthcare providers to detect any changes in liver function early and adjust the treatment plan as necessary. It's also important for patients to be aware of the potential risks and to report any new or worsening symptoms promptly.
Conclusion: The Balance between Benefit and Risk
In conclusion, while amiloride can be a beneficial medication for many patients, its use in those with hepatic impairment must be carefully monitored. The balance between the benefits of the medication and the potential risks associated with impaired liver function is a delicate one that requires careful management.
As with any medication, the key is to weigh the potential benefits against the potential risks. For many patients with liver disease, amiloride can still be a valuable part of their treatment plan, as long as their liver function is closely monitored.



Joey Yap on 12 July 2023, AT 14:40 PM
When we think about medicines like amiloride, we’re really staring at the delicate negotiation between the body’s own chemistry and the interventions we introduce. The liver, as the central hub of metabolism, acts as a wise steward, deciding which compounds are transformed and which are expelled. If that steward is weakened, the balance shifts and we must tread carefully. In patients with hepatic impairment, the usual pathways for amiloride clearance become less predictable, prompting a need for vigilance. Studies have shown that while amiloride can still be effective, dosage adjustments are often required to avoid unwanted potassium retention. The risk isn’t just theoretical; clinicians have reported cases where unadjusted dosing led to mild hyperkalemia. From a philosophical standpoint, this underscores the principle that every therapeutic choice carries a reciprocal responsibility. It reminds us that medicine is not a one‑size‑fits‑all but a dialogue with each individual’s physiology. Moreover, the interplay between heart failure, hypertension, and liver disease creates a triad of concerns that must be managed simultaneously. Monitoring liver enzymes and electrolyte panels becomes a moral imperative, not merely a procedural step. Patients themselves should feel empowered to report any new fatigue, jaundice, or swelling, as these may signal altered drug handling. The literature suggests that with regular testing, amiloride can be administered safely even in moderate impairment. Yet when the liver is severely compromised, many experts advise either switching to an alternative diuretic or drastically reducing the dose. This cautious approach aligns with the broader ethic of “primum non nocere.” Ultimately, the goal is to preserve the therapeutic benefits while respecting the limits of a compromised organ. By staying attentive to the nuances of hepatic function, we honor both science and the lived experience of the patient.