When your liver is damaged over years-by alcohol, fatty liver, or hepatitis-it doesn’t just get sore. It turns scarred. This is cirrhosis: the final, irreversible stage of chronic liver disease. Healthy tissue is replaced by hard, fibrous bands that block blood flow and cripple function. By 2022, about 600,000 Americans were living with it. Around 31,000 died from it that year alone. And for many, the worst isn’t the disease itself-it’s what comes next.
What Happens When Cirrhosis Gets Worse?
Cirrhosis has two stages: compensated and decompensated. In compensated cirrhosis, your liver is scarred but still doing enough to keep you alive. You might feel tired or lose weight, but you can still work, cook, and take care of yourself. Once you cross into decompensated cirrhosis, things change fast. Your body starts to break down. The first major sign? Fluid buildup in your belly-ascites. This isn’t just bloating. It’s pressure. It makes breathing hard. It can get infected, leading to spontaneous bacterial peritonitis, which kills 20-40% of people who get it during hospitalization. Managing ascites means cutting salt to under 2 grams a day and taking diuretics like spironolactone. But 1 in 10 people don’t respond. They need a needle inserted into their abdomen to drain liters of fluid-up to 16,000 times a year in the U.S. alone. Then there’s portal hypertension. Scar tissue squeezes the veins leading into your liver. Pressure builds. Blood finds other paths-through fragile veins in your esophagus and stomach. These are varices. They’re like time bombs. When they burst, you bleed. Up to 35% of people with cirrhosis will have this happen. Mortality per bleed? 15-20%. Even with banding and beta-blockers like propranolol, 60% rebleed within a year if not properly managed. Your brain suffers too. Hepatic encephalopathy is when toxins your liver can’t filter build up and fog your thinking. You forget names. You get confused. You might slur words or sleep all day. It affects 30-45% of those with decompensated cirrhosis. Lactulose helps-cutting recurrence in half-but the side effects are brutal. One patient on Reddit said, “The constant diarrhea makes social life impossible-I’ve missed 12 family events this year.” And then there’s cancer. Hepatocellular carcinoma (HCC) develops in 2-8% of cirrhotic patients every year. That’s why every single person with cirrhosis needs an ultrasound every six months. Screening finds tumors early-when they’re still small and treatable. Without it, 70% of cancers are found too late.How Doctors Measure How Bad It Is
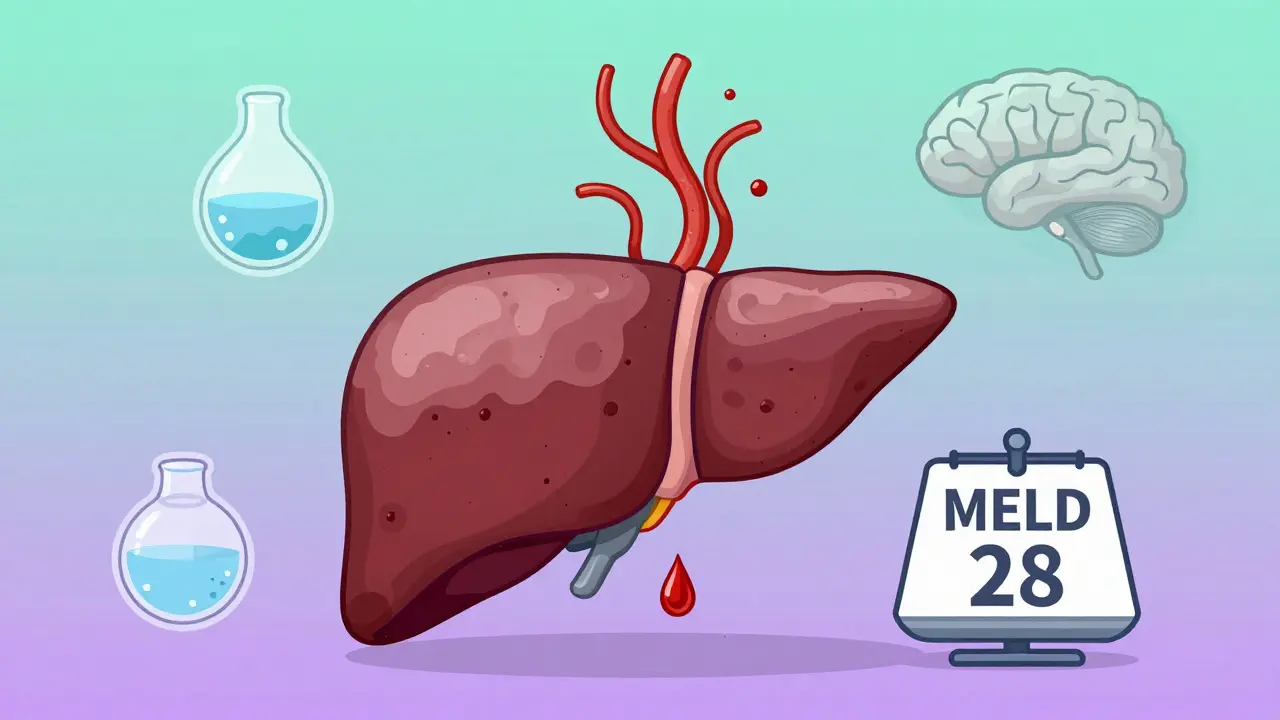
Not all cirrhosis is the same. Two people with the same diagnosis can have wildly different outlooks. That’s why doctors use scoring systems. The Child-Pugh score looks at five things: bilirubin, albumin, INR, ascites, and brain function. Class A (5-6 points) means a 100% chance of surviving one year. Class C (10-15 points)? Only 45%. That’s the difference between managing at home and needing a transplant next month. The MELD score is even more precise. It uses creatinine, bilirubin, and INR to predict death risk within 90 days. A score of 15 or higher means high risk. It’s used to prioritize who gets a liver transplant first. But here’s the problem: someone with frequent confusion from encephalopathy might have a low MELD score but be suffering more than someone with a higher score. Their quality of life is worse. Experts are pushing to change the system to include quality-of-life factors-and in February 2024, the organ allocation system finally started doing that.How to Treat the Complications
There’s no magic cure for cirrhosis. But there are proven ways to slow it, prevent disasters, and keep people alive longer. For varices: non-selective beta-blockers like propranolol or nadolol reduce bleeding risk by 45%. Carvedilol works even better-it lowers pressure in the liver’s veins more than other drugs. You don’t just take them; you monitor your heart rate and blood pressure closely. For ascites: albumin infusions after large paracentesis drop the risk of circulatory collapse from 37% to just 10%. It’s simple, effective, and standard now. For hepatic encephalopathy: rifaximin (550 mg twice daily) cuts hospital visits by 58%. It’s expensive-$1,200 a month without insurance-but it works. And for people who can’t tolerate lactulose, it’s a lifeline. For liver cancer: biannual ultrasounds are non-negotiable. Add a blood test for AFP (alpha-fetoprotein) if your doctor recommends it. Catching HCC early means surgery or ablation is still possible. Miss it, and transplant may be the only option.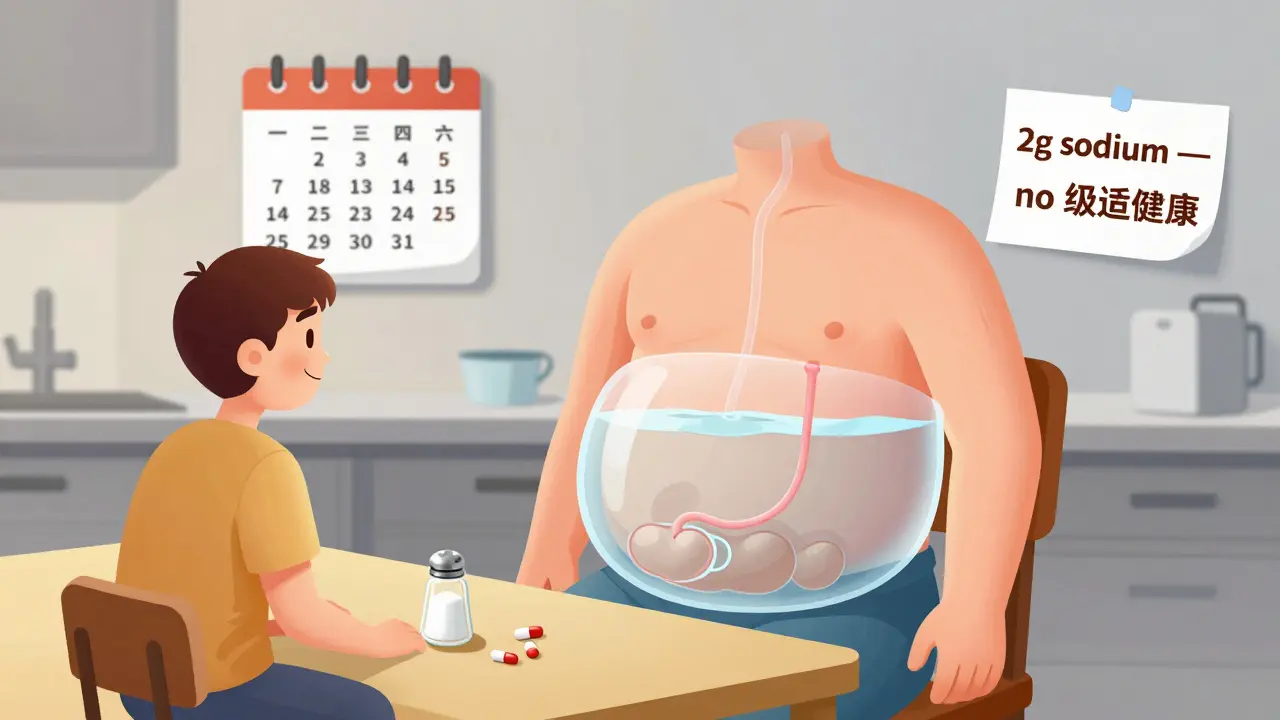
What’s New in Treatment?
The field is moving fast. In March 2024, the FDA approved resmetirom (Rezdiffra) for MASH-related cirrhosis. In clinical trials, it reduced liver fibrosis in over 20% of patients after a year. That’s huge. For the first time, we have a drug that doesn’t just manage symptoms-it might actually reverse scarring. Artificial intelligence is stepping in too. An algorithm called CirrhoPredict, tested in 2024, can predict which patients will decompensate in the next 90 days with 88% accuracy-just from routine blood tests. Imagine catching a flare-up before you even feel sick. And the transplant system is changing. The new Continuous Distribution Framework doesn’t just look at how sick you are-it also considers how much your life has been ruined by cirrhosis. That’s a big shift. It’s not just about survival. It’s about living.What Patients Really Deal With
Behind every number is a person. A 2023 survey by the American Liver Foundation found 78% of cirrhosis patients had fatigue so bad it stopped them from working or doing chores. 65% described “brain fog” so thick they couldn’t follow conversations or remember appointments. One woman said, “I used to be a teacher. Now I can’t even help my grandkids with homework.” Hospital visits for paracentesis? 42% of patients needed one every three months. And 73% said the pain was at least a 5 out of 10. No one talks about how draining that is-not just physically, but emotionally. But there’s hope. People who get transplants often say they feel reborn. One patient posted: “18 months post-transplant, my MELD score dropped from 28 to 9. I went back to full-time work.” That’s not just survival. That’s living again.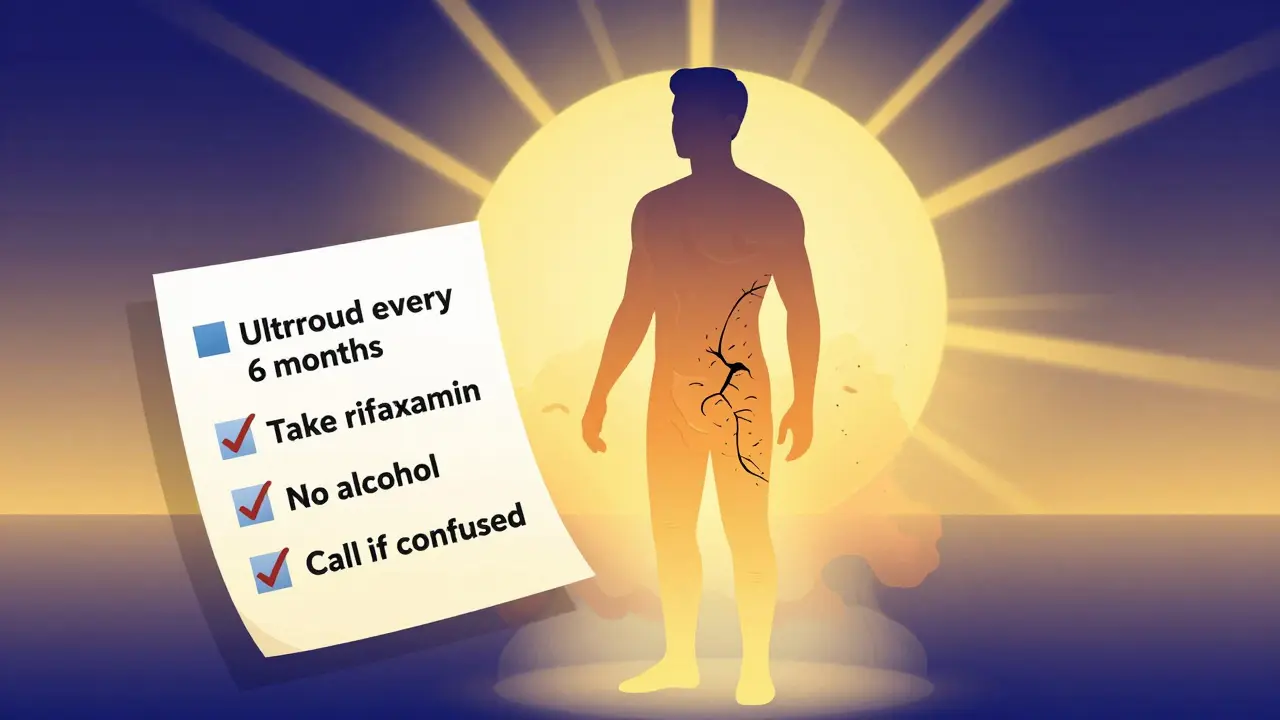
How to Stay Out of the Hospital
The best way to avoid complications? Structure. - See your hepatologist monthly if you’re decompensated. Quarterly if you’re stable. - Meet with a dietitian. A 2-gram sodium diet isn’t a suggestion-it’s medical treatment. - Get vaccinated. Hepatitis A and B, flu, pneumonia-every shot matters. - Quit alcohol. No exceptions. Even if your cirrhosis started from fatty liver, alcohol speeds death. - Take your meds. A study showed that with nurse-led follow-ups, medication adherence jumped from 62% to 85%. That cut ER visits by 40%. - Monitor your weight daily. A 2-pound gain in a day? That’s fluid. Call your doctor.When to Think About a Transplant
A transplant isn’t a last resort. It’s the best option for many with decompensated cirrhosis. But you have to start early. You should be evaluated if:- Your MELD score is 15 or higher
- You’ve had one or more episodes of variceal bleeding
- You have recurrent hepatic encephalopathy that won’t stabilize
- You’ve developed hepatocellular carcinoma within transplant criteria
Final Thoughts
Cirrhosis isn’t a death sentence. But it’s not something you can ignore. It demands daily attention. It requires discipline. It needs a team-doctors, nurses, dietitians, social workers. The good news? We’re getting better. New drugs. Better screening. Smarter allocation. More compassion in care. The next decade could see 40% of early cirrhosis reversed with new therapies. But right now, the most powerful tool you have is knowing the signs. Acting fast. Sticking to the plan. And never letting anyone tell you that your suffering doesn’t matter.What are the first signs of cirrhosis?
Early signs include fatigue, unintentional weight loss, easy bruising, swelling in the legs or abdomen, and itching. These are often mistaken for normal aging or stress. But if you have a history of heavy drinking, obesity, or hepatitis, these symptoms shouldn’t be ignored. See a doctor for a liver ultrasound or FibroScan.
Can cirrhosis be reversed?
In its earliest stages, before severe scarring sets in, stopping the cause-like alcohol or fatty liver-can allow the liver to heal partially. New drugs like resmetirom show promise in reversing fibrosis in MASH-related cirrhosis. But once nodules and dense scar tissue form, it’s irreversible. The goal then is to stop progression and prevent complications.
How often should I get screened for liver cancer if I have cirrhosis?
Every six months. That means an ultrasound and sometimes a blood test for AFP. This isn’t optional. Screening catches tumors when they’re small and treatable. Without it, most cancers are found too late for surgery or ablation. The survival rate jumps from 30% to 70% with regular screening.
Is it safe to take over-the-counter painkillers with cirrhosis?
No. Avoid NSAIDs like ibuprofen and naproxen-they can cause kidney damage and worsen fluid retention. Acetaminophen (Tylenol) is safer but should be limited to 2,000 mg per day. Always check with your doctor before taking any medication, even supplements. Your liver can’t process them like it used to.
What’s the difference between MELD and Child-Pugh scores?
Both measure liver function, but MELD is more accurate for predicting short-term death risk and is used to prioritize transplant candidates. Child-Pugh is simpler and used more for general prognosis and treatment planning. MELD uses creatinine, bilirubin, and INR. Child-Pugh adds albumin, ascites, and brain function. Doctors use both together to get the full picture.
Can I still work if I have cirrhosis?
Many people can, especially in compensated cirrhosis. But fatigue and brain fog make it harder. Some switch to part-time roles or remote work. If you have ascites or frequent hospital visits, you may need disability support. Don’t push through exhaustion-it can trigger decompensation. Talk to your doctor about accommodations and your rights under the ADA.
What should I do if I start feeling confused or forgetful?
That’s a red flag for hepatic encephalopathy. Call your doctor immediately. Don’t wait. Start lactulose if you’ve been prescribed it. Avoid protein-heavy meals for 24 hours. Get checked for infections, constipation, or electrolyte imbalances-all of which can trigger confusion. Early treatment can reverse it. Delayed treatment can lead to coma.
Is liver transplant the only option for end-stage cirrhosis?
It’s the only cure. But not everyone is a candidate. You must be healthy enough for major surgery, free from active infection or cancer outside the liver, and committed to lifelong care. Some patients with recurrent encephalopathy or severe frailty may not qualify. New therapies may change this in the future, but for now, transplant remains the only way to restore normal liver function.


Edith Brederode on 19 January 2026, AT 03:19 AM
This post hit me right in the feels. 😭 I’ve been watching my mom go through this for two years. The ascites alone? She’s had 12 paracenteses. I used to think ‘just cut the salt’ was easy-until I saw her cry because she couldn’t eat her favorite soup. 🥲 But we’re on rifaximin now, and her brain fog’s improved. Still, the loneliness is worse than the pain.