Why Checking Active Ingredients Saves Lives
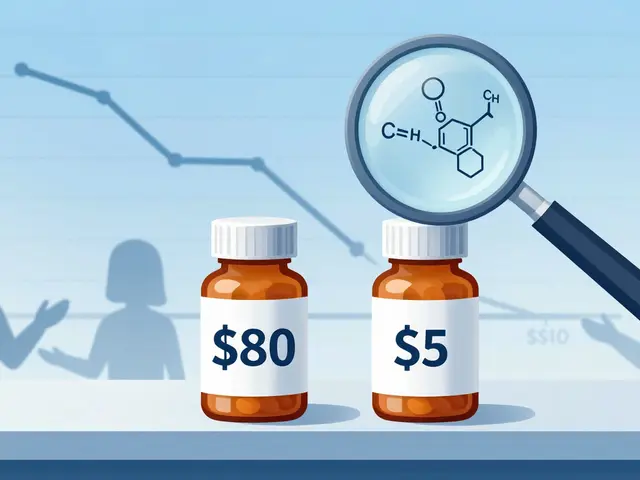
Every year, thousands of children end up in emergency rooms because their parents gave them two medicines that looked different but contained the same medicine inside. It’s not a mistake made by careless parents-it’s a trap built into how medicines are sold. A child gets a cough syrup. Later, they get a fever reducer. Both are labeled for kids. Both smell sweet. Both are in the same medicine cabinet. But both contain acetaminophen. And together, they’re too much.
According to the CDC, nearly 7 out of 10 pediatric medication overdoses happen because parents didn’t realize two different bottles had the same active ingredient. This isn’t rare. It’s common. And it’s preventable.
What’s in Your Medicine Cabinet?
Most over-the-counter kids’ medicines aren’t just one thing. They’re combinations. A cold medicine might have acetaminophen for fever, dextromethorphan for cough, and diphenhydramine for runny nose. But if you give that and then give a separate fever reducer, you’re doubling up-without even knowing it.
Here’s what you need to know about the most dangerous ingredients:
- Acetaminophen (also called paracetamol, APAP, or N-acetyl-p-aminophenol): Found in Tylenol, Panadol, Children’s NyQuil, Theraflu, Vicks DayQuil, and more. Too much can cause liver failure. Just 150 mg per kg of body weight can be toxic.
- Ibuprofen: Found in Advil, Motrin, and many cold/flu combos. Too much can damage kidneys or cause stomach bleeding.
- Diphenhydramine: Found in Benadryl, Children’s NyQuil, and some cough syrups. Too much causes extreme drowsiness, confusion, or even seizures.
- Phenylephrine and Pseudoephedrine: Decongestants in cold medicines. Can raise heart rate and blood pressure dangerously in small children.
Here’s the scary part: 89% of multi-symptom cold medicines contain acetaminophen. And 73% of parents don’t realize it’s in more than one product. If your child is on a prescription for ADHD medication like Adderall or Ritalin, mixing it with a cold medicine that has decongestants can spike heart rate and blood pressure fast-sometimes within 30 minutes.
How to Avoid Double Dosing
There’s no magic trick. No app that fixes everything. But there is a simple, free habit that cuts your risk by more than half:
- Look at the front of every bottle. Don’t just read the brand name. Look for the section that says “Active Ingredients.”
- Write it down. Keep a list on your phone or a sticky note: “NyQuil = acetaminophen, dextromethorphan, doxylamine.” “Tylenol = acetaminophen.” “Benadryl = diphenhydramine.”
- Never mix unless you’re sure. If you’re giving two medicines, check: Do they share an active ingredient? If yes, skip one.
- One person gives the meds. If two caregivers are involved, assign one person to handle all doses. Communication errors cause 38% of double dosing incidents.
- Use only the measuring tool that comes with the medicine. A kitchen teaspoon can hold anywhere from 2.5ml to 7.5ml. The FDA says this is why some kids get triple doses by accident.
One parent on Reddit shared how their 4-year-old ended up in the ER after getting Benadryl for allergies and then a cough syrup with the same ingredient. The child was so sleepy they couldn’t wake up. That could’ve been avoided with 10 seconds of checking the bottle.

What to Do If You Accidentally Double Dose
If you realize you gave too much:
- Don’t wait for symptoms. Call Poison Control immediately at 1-800-222-1222. They’re free, available 24/7, and trained for this exact situation.
- Have the medicine bottle ready. They’ll need the active ingredient, strength, and how much was given.
- Don’t try to make them throw up. That can make things worse.
- Don’t assume it’s fine because they seem okay. Acetaminophen damage can take 24-48 hours to show up. By then, it’s too late.
Emergency rooms see 32% of all pediatric medication overdoses as acetaminophen-related. Half of those cases need a special antidote called N-acetylcysteine. If you act fast, treatment works. If you wait, it can mean liver failure.
What’s Changing to Help Parents
Things are slowly getting better. In 2024, the American Academy of Pediatrics launched the “Know Your Ingredients” campaign, putting simple icons on medicine boxes so you can spot acetaminophen at a glance. By December 2025, the FDA will require all children’s OTC medicines to list active ingredients in bold, standardized format-no more hiding them in tiny print.
Some companies are adding QR codes that link to ingredient breakdowns. Amazon Pharmacy now scans your purchases and warns you if you’re buying two medicines with the same active ingredient. In pilot programs, this has prevented 12,000 potential overdoses in just six months.
But technology won’t fix everything. The biggest change comes from you. When you learn to read the back of the bottle before you give it to your child, you become the most important safety system they have.

Real Stories, Real Results
One dad, who goes by “PharmDad” on BabyCenter, started keeping a printed “medication map” after his 2-year-old accidentally got two doses of acetaminophen. He listed every medicine in the house, its active ingredient, and when it was last given. Within six months, his family had zero dosing errors.
Another mom, after her child’s ER visit, started asking pharmacists: “Is this the same as what’s in the other bottle?” She says it changed everything. “I used to think if it looked different, it was different. Now I know: same ingredient, same risk.”
Studies show parents who get just 10 minutes of focused instruction on active ingredients reduce their dosing errors from 42% to 12%. That’s not luck. That’s knowledge.
What Not to Do
Here are common mistakes that put kids at risk:
- Alternating acetaminophen and ibuprofen for fever: The American Academy of Family Physicians says this increases double dosing risk by 47%. Stick to one.
- Using flavor as a guide: “Orange tastes stronger, so I gave less.” No. Flavor doesn’t change strength. 120mg/5ml is 120mg/5ml, no matter the color.
- Assuming “children’s” means safe to mix: Just because it says “for kids” doesn’t mean it’s safe with other kids’ meds.
- Not checking long-acting versions: Extended-release ADHD meds stay in the body for up to 72 hours. Giving another dose too soon can be deadly.
Final Checklist Before Giving Any Medicine
Before you open a bottle, ask yourself:
- Is this medicine already in my child’s system from another product?
- What’s the active ingredient? (Look at the label-not the brand name.)
- Is the dose based on weight? (If yes, double-check the chart.)
- Am I using the right measuring tool?
- Who gave the last dose? When?
If you can’t answer all five, stop. Call your pharmacist. Call Poison Control. Wait. Double-check. Better safe than sorry.
What should I do if I think my child got too much medicine?
Call Poison Control at 1-800-222-1222 right away. Have the medicine bottle in hand so you can tell them the active ingredient, how much was given, and when. Don’t wait for symptoms. Don’t try to make them vomit. Don’t assume it’s fine because they seem okay. Acetaminophen overdose, for example, can damage the liver without showing signs for hours.
Can I give my child both Tylenol and a cold medicine that has acetaminophen?
No. Tylenol and most cold medicines like Children’s NyQuil, Vicks DayQuil, and Theraflu all contain acetaminophen. Giving both together can easily lead to a dangerous overdose. Choose one medicine that treats your child’s symptoms. If you’re unsure, ask your pharmacist or doctor.
Why do some medicine labels say “acetaminophen” and others say “paracetamol”?
They’re the same thing. Acetaminophen is the name used in the U.S. Paracetamol is used in many other countries, including Australia and the UK. APAP on labels also means acetaminophen. If you see any of these three, treat them as identical. Don’t give more than one.
Are liquid medicines safer than pills for kids?
Liquid medicines are easier to dose for small children, but they’re also riskier because measuring errors are common. A kitchen spoon can hold 2 to 3 times more than a proper measuring cup. Always use the dropper, syringe, or cup that comes with the medicine. Never guess.
Should I alternate ibuprofen and acetaminophen for fever?
No. The American Academy of Family Physicians advises against this for children under 3. It increases the chance of double dosing by nearly 50%. Stick with one medicine and use it as directed. If the fever doesn’t come down, talk to your doctor-not your medicine cabinet.
What if my child is on a prescription medication like Adderall or insulin?
Be extra careful. Adderall and other stimulants can interact dangerously with decongestants found in cold medicines, raising heart rate and blood pressure fast. Insulin overdoses can cause life-threatening low blood sugar. Always check with your child’s doctor before giving any OTC medicine alongside a prescription.



Brian Bell on 13 November 2025, AT 04:50 AM
This is literally life-saving info. I had no idea so many cold meds had acetaminophen. I just gave my kid Tylenol and a cough syrup last week... 🤦♂️