Antibiotic Decision Tool
Choose Your Scenario
Select your clinical scenario to get personalized antibiotic recommendations
Select your scenario to see recommendations
Quick Summary
- Minocin (minocycline) is a broad‑spectrum tetracycline often chosen for acne and certain infections.
- Its main rivals include doxycycline, tetracycline, amoxicillin, azithromycin and clindamycin.
- Minocin offers better tissue penetration but carries higher risk of vestibular side effects.
- Choosing the right alternative depends on infection type, patient age, pregnancy status and drug‑interaction profile.
- Monitoring liver function and sun exposure is crucial for all tetracyclines.
When you see a prescription for Minocin (Minocycline) is a semi‑synthetic tetracycline antibiotic that blocks bacterial protein synthesis by binding to the 30S ribosomal subunit. It was launched in the 1970s and quickly became a go‑to for moderate to severe acne, certain skin infections, and some tick‑borne diseases like Lyme disease. Its reputation comes from high lipid solubility, which lets it reach deep tissue and even the central nervous system.
How Minocin Works Compared to Other Classes
All tetracyclines share a core mechanism: they prevent bacteria from adding new amino acids to growing proteins. That stops bacterial growth without killing the host cells. However, each drug differs in absorption, half‑life, and side‑effect profile.
Below is a snapshot of the most common alternatives and where they diverge from Minocin.
| Attribute | Minocin (Minocycline) | Doxycycline | Tetracycline | Amoxicillin | Azithromycin | Clindamycin |
|---|---|---|---|---|---|---|
| Drug class | Tetracycline | Tetracycline | Tetracycline | Penicillin‑type | Macrolide | Lincosamide |
| Typical dose (adult) | 100 mg twice daily | 100 mg twice daily | 250-500 mg four times daily | 500 mg three times daily | 500 mg once daily (or 250 mg twice daily) | 300 mg three times daily |
| Half‑life | ≈ 16 h | ≈ 18 h | ≈ 8 h | ≈ 1 h | ≈ 68 h | ≈ 2.5 h |
| Common uses | Acne, rosacea, Lyme disease, MRSA skin infections | Acne, chlamydia, travel‑related fever | Broad‑spectrum bacterial infections | Otitis media, sinusitis, streptococcal pharyngitis | Community‑acquired pneumonia, gonorrhea, skin infections | Severe anaerobic infections, bone‑joint infections |
| Key side effects | Vertigo, vestibular disturbances, hyperpigmentation, photosensitivity | Photosensitivity, GI upset | Photosensitivity, GI upset | Allergic rash, GI upset | QT prolongation, GI upset | C. difficile infection, GI upset |
| Pregnancy safety | Category D - avoid unless essential | Category D - avoid unless essential | Category D - avoid unless essential | Category B - generally safe | Category B - generally safe | Category B - generally safe |
When Minocin Is the Top Choice
Minocin shines in three scenarios:
- Acne that hasn’t responded to doxycycline or topical therapy. Its better penetration into sebaceous glands can reduce inflammatory lesions faster.
- Neurologic manifestations of Lyme disease, such as facial palsy, because it crosses the blood‑brain barrier more efficiently than doxycycline.
- Infections caused by resistant Staphylococcus aureus where other tetracyclines fail. Some studies from 2023 show Minocin retains activity against strains resistant to doxycycline.
Even with these strengths, you must weigh the increased risk of dizziness and skin discoloration, especially in patients who already have balance problems.

Why You Might Prefer an Alternative
These alternatives win on specific fronts:
- Doxycycline has a similar spectrum but a lower incidence of vestibular side effects, making it a safer first‑line for acne in teenagers.
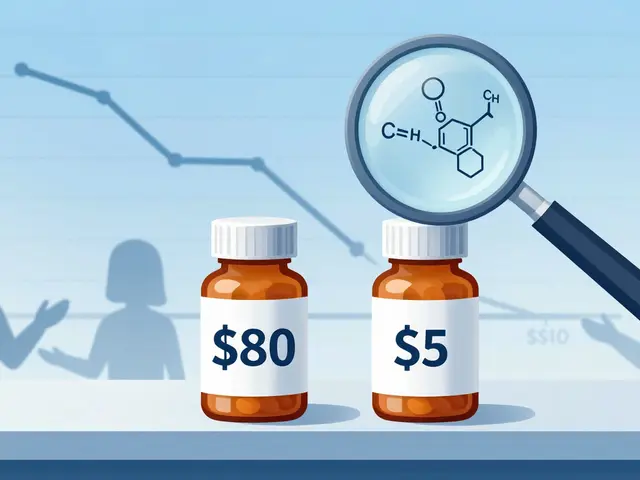
- Tetracycline is cheaper and widely available as a generic, suitable for short‑term travel‑related infections.
- Amoxicillin is the go‑to for respiratory and ear infections, especially in children, because it’s well‑tolerated and safe in pregnancy.
- Azithromycin offers a once‑daily dosing schedule and a long half‑life, useful for patients who struggle with adherence.
- Clindamycin is preferred for deep‑tissue anaerobic infections and certain bone infections where penicillins fail.
Choosing among them hinges on the infection type, patient comorbidities, and how the drug is metabolized.
Safety Concerns to Keep in Mind
All tetracyclines share a warning about photosensitivity. Patients should use sunscreen and wear protective clothing when outdoors. Minocin adds a few extra red flags:
- Vertigo and dizziness can impair driving - advise caution for anyone operating machinery. \n
- Rare but serious autoimmune hepatitis has been reported; liver function tests are advisable for prolonged courses.
- Hyperpigmentation of skin, teeth (in children) and scar tissue can occur, especially after 3+ months of therapy.
For patients with a history of C. difficile infection, clindamycin might be avoided, while macrolides like azithromycin carry a lower risk of this complication.
Practical Decision Tree
Use the flow below to narrow down the optimal antibiotic.
- Is the infection bacterial and known to be susceptible to tetracyclines?
- Yes → Continue to step 2.
- No → Consider non‑tetracycline agents (e.g., amoxicillin, azithromycin).
- Is the patient pregnant or planning pregnancy?
- Yes → Avoid Minocin, doxycycline, tetracycline; choose amoxicillin or azithromycin.
- No → Continue to step 3.
- Does the patient have a history of vestibular disorders or needs to drive frequently?
- Yes → Prefer doxycycline or azithromycin.
- No → Minocin remains a strong candidate.
- Is the infection deep‑tissue or CNS‑related (e.g., Lyme disease neurological involvement)?
- Yes → Minocin’s better CNS penetration makes it preferable.
- No → Evaluate cost, duration, and side‑effect tolerance.
Key Takeaways for Clinicians and Patients
- Minocin offers superior tissue penetration but brings vestibular side effects and pigmentation risks.
- Doxycycline is the safest first‑line tetracycline for acne and travel‑related infections.
- For pregnant patients, shift to amoxicillin or azithromycin.
- Always counsel on sun protection regardless of the tetracycline used.
- Monitor liver enzymes for long courses of Minocin and watch for signs of C. difficile with clindamycin.
Can I use Minocin for acne if I’m already on doxycycline?
Switching is possible when acne doesn’t improve after 8‑12 weeks of doxycycline. Minocin’s higher skin concentration can break the plateau, but you should taper off doxycycline to avoid overlapping side effects.
Is Minocin safe for children?
It’s generally avoided in children under 8 because of permanent tooth discoloration. In rare cases where the infection is severe and no alternative works, a pediatric infectious‑disease specialist may consider short‑term use.
How long should I stay on Minocin for Lyme disease?
Typical courses last 4‑6 weeks for early disseminated disease, extending to 8 weeks for neurologic involvement. Blood tests and symptom monitoring guide duration.
What should I do if I feel dizzy on Minocin?
Stop the medication and contact your doctor immediately. They may lower the dose, switch to doxycycline, or add antihistamine support, depending on severity.
Are there any drug interactions with Minocin?
Yes. Antacids, calcium, magnesium, and iron supplements can reduce absorption. Take Minocin at least 2 hours before or after these agents. Also, avoid concurrent use with warfarin without monitoring INR.



Erik Redli on 26 October 2025, AT 12:10 PM
Minocin’s supposed superiority is a myth-doxycycline gives the same coverage without the dizzy side‑effects.