Ulcers — what they are and what to do about them
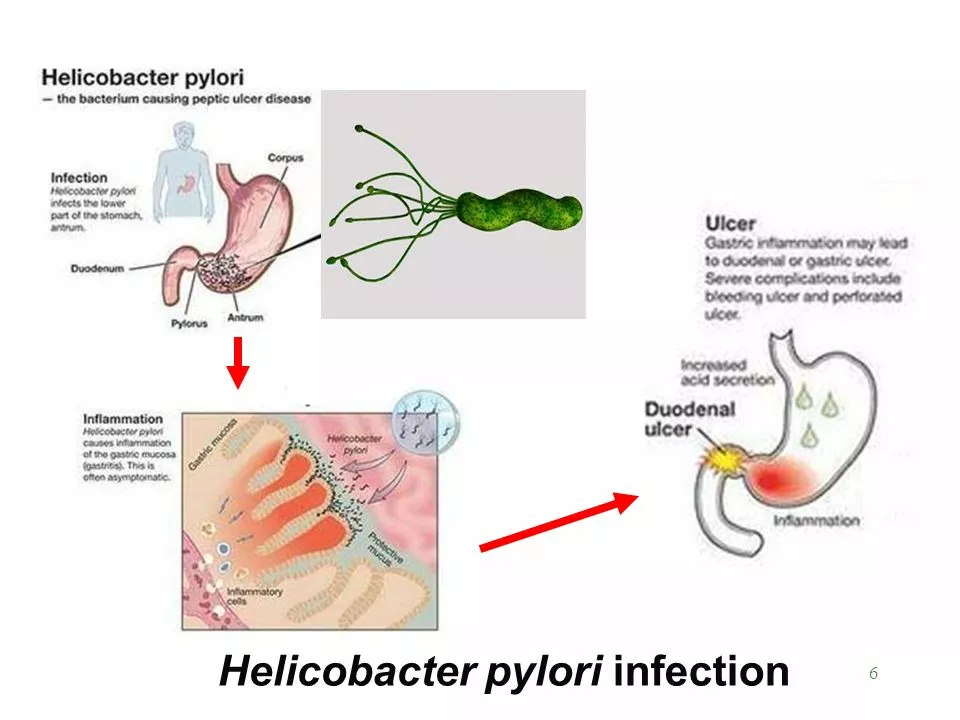
Think ulcers are caused by spicy food? Not exactly. Most ulcers come from H. pylori infection, everyday painkillers (NSAIDs), poor blood flow, or pressure and diabetes. Different ulcers need different fixes, so spotting the type early makes treatment simpler and faster.
Quick checklist: types, common causes, and symptoms
Peptic ulcers (stomach or duodenal): burning or gnawing belly pain, worse on an empty stomach, sometimes nausea, bloating or dark stools if bleeding. Major causes: H. pylori bacteria, long-term NSAID use (ibuprofen, naproxen), and some blood thinners.
Mouth ulcers: small painful sores on the gums or tongue. Often from minor injury, acid foods, low B12/iron, or viral infections.
Skin ulcers (pressure, venous, diabetic): open wounds that won’t heal, often on heels, ankles, or where bone presses the skin. Look for swelling, foul smell, increased pain, or dead tissue — these need fast care.
Practical steps you can take today
If you suspect a peptic ulcer: stop NSAIDs and talk to your doctor. They may test for H. pylori (breath or stool test) and prescribe antibiotics plus a PPI (proton pump inhibitor) to heal the lining. Don’t try to self-treat bleeding or severe pain — seek urgent care.
For mouth ulcers: avoid hot, salty, or acidic foods. Use topical gels or salt rinses for short-term relief. If ulcers return often, ask your doctor about blood tests for vitamin deficiencies or celiac disease.
For skin ulcers: keep the area clean, avoid pressure (use cushions or special shoes), and change dressings as advised. Diabetics must control blood sugar and see a wound clinic early — infections can spread fast.
Simple diet and habit tips that help heal faster: stop smoking, limit alcohol, eat balanced meals with protein and vitamin C for tissue repair, and stay hydrated. Spicy food might irritate symptoms but isn’t the root cause.
When to see a doctor right away: vomiting blood, black/tarry stools, sudden severe abdominal pain, fever with a skin ulcer, spreading redness, pus, or a wound that won’t improve after a few days of home care.
Want a deeper read? Check our related pieces on wound-friendly herbs like "Buck's-Horn Plantain Supplements" and digestive issues in "Keto Diet and Erosive Esophagitis." We also cover fungal and resistant infections that can complicate ulcers in other articles.
Bottom line: identify the type, remove obvious causes (like NSAIDs or pressure), use targeted treatments (antibiotics for H. pylori, PPIs for acid control, dressings/offloading for skin ulcers), and get medical help for bleeding, spreading infection, or non-healing wounds.
I recently came across some fascinating research that showed a connection between ulcers and a bacteria called Helicobacter pylori. It turns out that this bacteria is responsible for a majority of stomach ulcers, contrary to the popular belief that stress and spicy food cause them. H. pylori infection can be treated with antibiotics, which can help heal the ulcers and prevent their recurrence. I'm relieved to know that this new understanding of ulcers can lead to more effective treatments for those who suffer from them. It's amazing how medical science continues to uncover new information and improve our lives!