Anxiety Medication Comparison Tool
Select an anxiety medication or treatment approach below to see its key characteristics and compare it with others.
Buspirone
Mechanism: Serotonin-2A partial agonist
Onset: 1-2 weeks
Side Effects: Dizziness, nausea
Abuse Potential: Minimal
Best For: Generalized anxiety, long-term use
Escitalopram (SSRI)
Mechanism: Serotonin reuptake inhibition
Onset: 2-4 weeks
Side Effects: Sexual dysfunction, GI upset
Abuse Potential: None
Best For: Chronic anxiety, depression comorbidity
Alprazolam (Benzodiazepine)
Mechanism: GABA-A positive allosteric modulator
Onset: 30-60 min
Side Effects: Sedation, memory lapses
Abuse Potential: High
Best For: Panic attacks, short-term crisis
Hydroxyzine
Mechanism: H1 antihistamine with central effects
Onset: 15-30 min
Side Effects: Drowsiness, dry mouth
Abuse Potential: Low
Best For: Acute anxiety when benzodiazepine avoidance is desired
Gabapentin
Mechanism: Calcium channel modulation
Onset: 1-2 weeks
Side Effects: Swelling, dizziness
Abuse Potential: Moderate
Best For: Anxiety with neuropathic pain or alcohol withdrawal
CBT (Therapy)
Mechanism: Cognitive restructuring & exposure
Onset: Weeks-months
Side Effects: None
Abuse Potential: None
Best For: Long-term skill building, relapse prevention
Key Decision Points
- Speed of Relief: Alprazolam and Hydroxyzine act fastest (minutes to hours)
- Safety & Dependence Risk: Buspirone, SSRIs, and CBT have minimal risk
- Long-Term Use: Buspirone and SSRIs are well-suited for extended therapy
- Non-Drug Options: CBT offers skills without medication
Which Option Is Best For You?
Consider these factors when choosing your anxiety treatment:
- How quickly do you need relief? Fast-acting options like benzodiazepines or antihistamines are best for acute episodes.
- Are you concerned about dependence? Non-addictive options such as Buspirone or SSRIs are safer for long-term use.
- Do you have any medical conditions? Certain medications may interact with other health issues.
- Are you open to therapy? Cognitive Behavioral Therapy provides lasting benefits beyond medication alone.
Always consult with a healthcare provider to determine the safest and most effective treatment plan tailored to your situation.
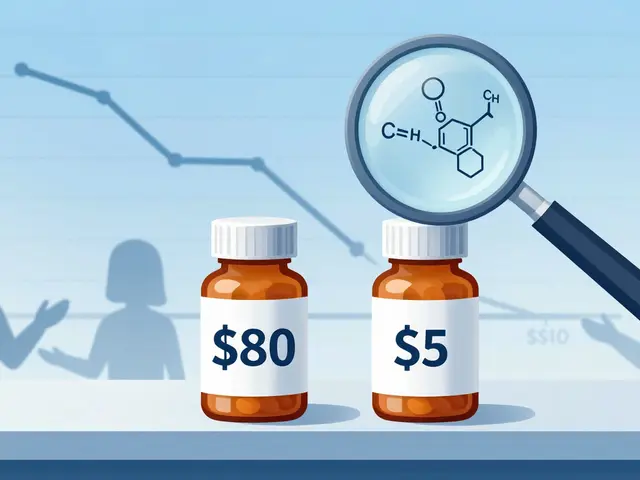
When you’ve tried to calm nerves with prescription pills, Buspirone often pops up as a non‑sedating option. But is it really the best fit, or do other drugs or even natural approaches work better for you? This guide breaks down how Buspirone works, weighs it against the most popular alternatives, and helps you decide which route matches your lifestyle and health profile.
Quick Takeaways
- Buspirone is a serotonin‑2A partial agonist; it takes 1‑2 weeks for full effect and carries minimal abuse risk.
- SSRIs (e.g., escitalopram) are first‑line for chronic anxiety but may cause sexual side effects.
- Benzodiazepines (e.g., alprazolam) work fast but are habit‑forming and unsuitable for long‑term use.
- Older antihistamines like hydroxyzine calm anxiety without dependence but can cause drowsiness.
- Herbal options (valerian, kava) offer mild relief for mild anxiety, yet evidence is mixed and liver safety is a concern.
How Buspirone Works
Buspirone is a non‑benzodiazepine anxiolytic that primarily targets serotonin‑2A receptors as a partial agonist. By modulating serotonin activity, it gradually reduces the physiological symptoms of anxiety without the heavy sedation associated with many other pills.
Key attributes:
- Onset: 7‑14 days for noticeable anxiety reduction.
- Typical dose: 5‑30mg split into two or three doses per day.
- Side‑effects: Light dizziness, headache, nausea; rare paradoxical agitation.
- Abuse potential: Near zero - it does not produce a “high.”
Because it needs time to build up, Buspirone is best for generalized anxiety disorder (GAD) that isn’t urgent or panic‑driven.
Major Alternatives to Consider
Escitalopram (SSRI)
Escitalopram belongs to the selective serotonin reuptake inhibitor class. It lifts mood by preventing serotonin reabsorption, making more of the neurotransmitter available in the brain. Most guidelines list SSRIs as first‑line for chronic anxiety.
Attributes:
- Onset: 2‑4 weeks.
- Typical dose: 5‑20mg daily.
- Side‑effects: Nausea, sexual dysfunction, insomnia.
- Abuse potential: None.
Alprazolam (Benzodiazepine)
Alprazolam enhances GABA activity, leading to rapid calming. It's often prescribed for acute panic attacks or short‑term relief.
Attributes:
- Onset: 30‑60 minutes.
- Typical dose: 0.25‑0.5mg three times daily as needed.
- Side‑effects: Sedation, memory issues, respiratory depression at high doses.
- Abuse potential: High - tolerance and dependence develop quickly.
Hydroxyzine (Antihistamine)
Hydroxyzine blocks H1 histamine receptors and also dampens central nervous system activity, offering a sedating but non‑addictive anxiolytic effect.
Attributes:
- Onset: 15‑30 minutes.
- Typical dose: 25‑100mg up to three times daily.
- Side‑effects: Drowsiness, dry mouth, mild anticholinergic effects.
- Abuse potential: Low; not scheduled.
Gabapentin (Neuropathic pain agent)
Although designed for seizures, gabapentin modulates calcium channels, reducing neuronal excitability, which can translate into anxiety relief for some patients.
Attributes:
- Onset: 1‑2 weeks.
- Typical dose: 300‑900mg three times daily.
- Side‑effects: Swelling, dizziness, possible misuse in high‑dose scenarios.
- Abuse potential: Moderate - some reports of off‑label recreational use.
Valerian root (Herbal)
Valerian is a plant extract often taken as a tea or capsule. It may increase GABA levels modestly, offering a calming effect for mild anxiety.
Attributes:
- Onset: 30‑60 minutes.
- Typical dose: 400‑900mg of standardized extract.
- Side‑effects: Headache, occasional vivid dreams.
- Abuse potential: Very low, but long‑term safety data are limited.
Kava (Herbal)
Kava contains kavalactones that act on GABA and dopamine receptors, producing relaxation. It’s popular in the Pacific Islands for ceremonial use.
Attributes:
- Onset: 1‑2 hours.
- Typical dose: 70‑250mg kavalactones daily.
- Side‑effects: Liver toxicity risk, especially with alcohol or acetaminophen.
- Abuse potential: Low, but safety concerns limit its use in many countries.
Cognitive Behavioral Therapy (CBT) (Non‑pharmacologic)
CBT teaches practical coping strategies, thought restructuring, and exposure techniques. While not a drug, it’s often combined with medication for lasting anxiety control.
Attributes:
- Onset: Weeks to months, depending on session frequency.
- Typical regimen: 12‑20 weekly sessions.
- Side‑effects: None; time commitment required.
- Abuse potential: None.

Side‑by‑Side Comparison
| Medication / Approach | Mechanism | Onset | Typical Dose | Key Side‑effects | Abuse Potential | Best For |
|---|---|---|---|---|---|---|
| Buspirone | Serotonin‑2A partial agonist | 1‑2 weeks | 5‑30mg split 2‑3×/day | Dizziness, nausea | Minimal | Generalized anxiety, long‑term use |
| Escitalopram (SSRI) | Serotonin reuptake inhibition | 2‑4 weeks | 5‑20mg daily | Sexual dysfunction, GI upset | None | Chronic anxiety, depression comorbidity |
| Alprazolam (Benzodiazepine) | GABA‑A positive allosteric modulator | 30‑60 min | 0.25‑0.5mg prn | Sedation, memory lapses | High | Panic attacks, short‑term crisis |
| Hydroxyzine | H1 antihistamine with central effects | 15‑30 min | 25‑100mg 2‑3×/day | Drowsiness, dry mouth | Low | Acute anxiety when benzodiazepine avoidance is desired |
| Gabapentin | Calcium channel modulation | 1‑2 weeks | 300‑900mg 3×/day | Swelling, dizziness | Moderate | Anxiety with neuropathic pain or alcohol withdrawal |
| Valerian root (Herbal) | GABA‑A facilitation (mild) | 30‑60 min | 400‑900mg extract | Headache, vivid dreams | Very low | Mild, situational anxiety |
| Kava (Herbal) | Kavalactones act on GABA & dopamine | 1‑2 hrs | 70‑250mg kavalactones | Liver toxicity risk | Low | Social anxiety, relaxation rituals |
| CBT (Therapy) | Cognitive restructuring & exposure | Weeks‑months | 12‑20 weekly sessions | None | None | Long‑term skill building, relapse prevention |
Choosing the Right Option for You
Ask yourself these four questions before settling on a treatment:
- How quickly do I need relief? If you need calm within an hour, a benzodiazepine or hydroxyzine wins. For steady, daily control, SSRIs or Buspirone are better.
- Am I worried about dependence? Buspirone, SSRIs, and CBT have negligible abuse risk. Benzodiazepines and high‑dose gabapentin carry more concern.
- Do I have medical conditions that limit certain drugs? Liver disease makes kava risky; heart arrhythmias can be worsened by some antihistamines.
- Can I commit to therapy? CBT demands time but often reduces or eliminates the need for medication.
When in doubt, start with the lowest‑risk option-often Buspirone for chronic GAD or hydroxyzine for short bursts-while arranging follow‑up with a prescriber.
Safety, Interactions, and Monitoring
Regardless of the choice, keep these safety tips in mind:
- Never combine multiple CNS depressants (e.g., benzodiazepines with alcohol or kava) without doctor approval.
- SSRIs may interact with certain migraine meds (triptans) and increase serotonin syndrome risk.
- Buspirone’s metabolism involves CYP3A4; grapefruit juice or strong inhibitors (ketoconazole) can raise blood levels.
- Regular liver function tests are recommended if you use kava or high‑dose valine.
- Track symptom changes weekly; adjust dose only after a steadied baseline (usually 2 weeks for Buspirone, 4 weeks for SSRIs).
Frequently Asked Questions
Can I switch from a benzodiazepine to Buspirone safely?
Yes, but do it gradually. Taper the benzodiazepine over weeks while introducing Buspirone at a low dose. Always do this under medical supervision to avoid withdrawal symptoms.
Is Buspirone effective for panic attacks?
Buspirone works best for generalized anxiety. For sudden panic attacks, fast‑acting agents like alprazolam or hydroxyzine are usually preferred.
Can I use Buspirone with antidepressants?
Combining Buspirone with SSRIs or SNRIs is common and generally safe. Monitor for dizziness or serotonin syndrome signs, though those are rare.
Are herbal options like valerian or kava legal in Australia?
Valerian is widely available as a supplement. Kava is restricted in some states due to liver concerns, so check local regulations before buying.
How long can I stay on Buspirone?
Because it has no dependence risk, many clinicians keep patients on Buspirone for years if it controls symptoms and side‑effects remain mild.

Next Steps
1. List your top priorities (speed, safety, cost).
2. Talk to a pharmacist or doctor about the options that align with those priorities.
3. If you start a new medication, set a reminder to review efficacy after the recommended onset period (e.g., 2 weeks for Buspirone).
4. Consider adding CBT or a mindfulness program to boost long‑term resilience.



Sukanya Borborah on 4 October 2025, AT 13:27 PM
The pharmacodynamic profile of buspirone, as delineated in the literature, underscores its role as a serotonin‑2A partial agonist, which inherently differentiates it from the GABAergic mechanisms of benzodiazepines. Its onset latency of one to two weeks, while seemingly protracted, aligns with the neuroadaptive processes required for serotonergic modulation. Moreover, the metabolic pathway via CYP3A4 introduces a notable drug‑interaction vector, particularly with potent inhibitors such as ketoconazole, a factor that clinicians must vigilantly monitor. The side‑effect spectrum-chiefly dizziness and nausea-is comparatively mild, especially when juxtaposed against the sexual dysfunction endemic to SSRIs. In terms of abuse potential, buspirone is virtually negligible, rendering it an attractive candidate for long‑term maintenance therapy without the specter of dependence. The dosing regimen, typically partitioned into two or three daily administrations, facilitates steady plasma concentrations, thereby optimizing therapeutic efficacy. From a cost‑effectiveness perspective, generic formulations are widely available, mitigating financial barriers for patients. Clinical guidelines frequently endorse buspirone as a second‑line agent for generalized anxiety disorder when SSRIs are contraindicated or poorly tolerated. It is also prudent to note that the absence of sedative properties distinguishes it from antihistaminergic agents like hydroxyzine, preserving daytime alertness. While the evidence base is robust, some meta‑analyses suggest modest effect sizes, prompting the need for individualized risk‑benefit assessments. Ultimately, the selection of buspirone should be contextualized within a comprehensive treatment plan that may incorporate psychotherapy, lifestyle modifications, and close monitoring of therapeutic response.