When you’re managing heart disease, diabetes, or high blood pressure, taking multiple pills every day isn’t just inconvenient-it’s a major reason why people stop taking their meds. Studies show that when patients have to swallow four or more pills daily, adherence drops to just 25-30%. But what if you could take one pill instead of four? That’s the promise of cardiovascular combination generics.
What Are Cardiovascular Combination Generics?
These are single pills that combine two or more cardiovascular drugs into one tablet. Think of them as a simplified version of your medicine cabinet. Instead of grabbing a blue pill for blood pressure, a white pill for cholesterol, and a red pill for blood thinning, you take one pill that does it all.
The idea isn’t new. Back in 2002, Dr. Salim Yusuf proposed the "polypill"-a single tablet containing aspirin, a beta-blocker, an ACE inhibitor, and a statin. His math showed it could slash cardiovascular events by 75% in people who’d already had a heart attack or stroke. Today, we’re not quite there yet in the U.S., but we’re getting close.
These combinations are made with generic versions of proven drugs: things like atorvastatin for cholesterol, lisinopril for blood pressure, metoprolol for heart rate, and aspirin to prevent clots. The FDA requires these generics to deliver the same amount of active ingredient as the brand name, within a strict 80-125% range. That’s not a guess-it’s science.
Why Do They Work Better Than Separate Pills?
It’s not magic. It’s simplicity.
Take a 68-year-old with high blood pressure, high cholesterol, and a history of heart attack. Without combination pills, they’re juggling:
- Atorvastatin 20 mg (morning)
- Lisinopril 10 mg (morning)
- Metoprolol 50 mg (twice daily)
- Aspirin 81 mg (evening)
That’s five pills a day. Now imagine one pill that combines atorvastatin and lisinopril, and another that has metoprolol and aspirin. That’s two pills. The pill burden drops by 60%. And guess what? Studies show adherence jumps from 55% to 75-85% when you cut the number of pills.
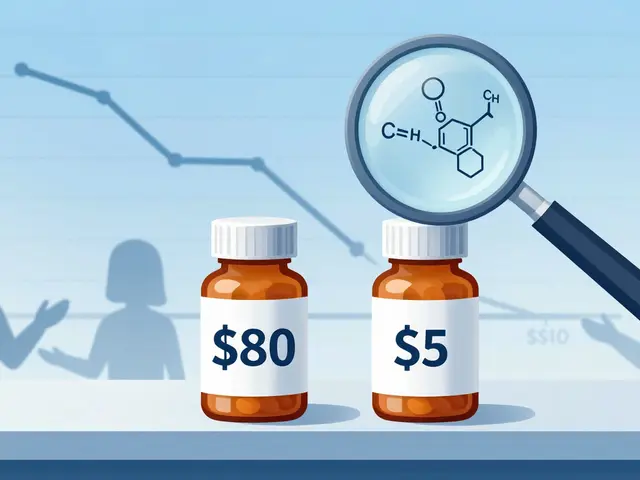
Medicare data from 2017 showed brand-name cardiovascular meds cost $85.43 per fill. Generic combinations? Around $15.67. That’s an 82% savings. Multiply that across millions of patients, and you’re looking at over $1 billion in annual savings-money that stays in patients’ pockets and reduces strain on the system.
What Combination Generics Are Actually Available?
Not every possible combo exists yet-but many do. Here’s what’s on the market in the U.S. as of 2025:
| Combination | Brand Name (Original) | Generic Availability | Typical Use |
|---|---|---|---|
| Atorvastatin + Amlodipine | Caduet | 2010 | High blood pressure + high cholesterol |
| Hydrochlorothiazide + Lisinopril | Zestoretic | 2008 | High blood pressure |
| Hydrochlorothiazide + Olmesartan | Benicar HCT | 2015 | High blood pressure |
| Simvastatin + Ezetimibe | Vytorin | 2016 | Cholesterol control |
| Carvedilol + Hydrochlorothiazide | Coreg HCT | 2014 | High blood pressure + heart failure |
| Losartan + Hydrochlorothiazide | Hyzaar | 2006 | High blood pressure |
| Metoprolol + Hydrochlorothiazide | Toprol-HCT | 2011 | High blood pressure |
| Sacubitril + Valsartan | Entresto | 2022 | Heart failure |
Some combos are newer. Entresto’s generic version hit the market in 2022-big news for heart failure patients. Before that, Entresto cost over $500 a month. Now, generics are under $30. That’s life-changing.
But here’s the catch: there’s no single pill yet that combines aspirin, a beta-blocker, an ACE inhibitor, and a statin-the full "polypill" Dr. Yusuf imagined. In places like India and the UK, they’ve rolled it out for high-risk patients. In the U.S., you still need two or three pills.
Are Generics Really as Good as Brand Names?
Yes. But not everyone believes it.
A 2014 review of 61 clinical trials in the European Heart Journal found no meaningful difference in effectiveness or safety between brand-name and generic cardiovascular drugs. The FDA’s bioequivalence standards are strict. If a generic doesn’t perform the same, it doesn’t get approved.
Still, 65% of pharmacists say patients worry about generics. The top fears? "Will it work?" and "Will I get side effects?"
On Drugs.com, 78% of 1,245 patients rated generic heart meds as "equally effective" as brand names. Only 12% reported noticeable side effect differences-mostly with beta-blockers or calcium channel blockers. Why? Sometimes it’s the inactive ingredients. A generic might use a different filler or coating. For most people, that’s harmless. But for someone with a rare allergy or a condition like epilepsy or heart failure, even tiny differences can matter.
Dr. Aaron Kesselheim from Brigham and Women’s Hospital warned in The New England Journal of Medicine that some high-risk patients-like those on warfarin or with advanced heart failure-need extra monitoring when switching. It’s not that generics are unsafe. It’s that transitions need care.
What Are the Alternatives If a Combo Isn’t Available?
Not every combo exists as a pill. But that doesn’t mean you’re stuck with a messy pillbox.
Here’s what you can do:
- Ask your doctor about individual generics. Even if you can’t get a combo pill, you can still get each component as a cheap generic. Lisinopril costs less than $5 a month. Atorvastatin? Under $10. Aspirin? Pennies.
- Use a pill organizer. A simple weekly pill box cuts confusion. Many pharmacies offer them free.
- Set phone reminders. A 2019 study found that daily text reminders improved adherence by 20% in older adults.
- Ask about mail-order pharmacies. They often sell 90-day supplies at lower prices, reducing refill frequency.
And if you’re on a combo that’s still brand-only-like metoprolol + hydrochlorothiazide-ask your doctor if switching to two separate generics would work. Sometimes, it’s cheaper and just as effective.
Why Aren’t These Combos Used More Often?
Because the system isn’t built for them.
A 2018 study found only 45% of primary care doctors knew all the available generic combinations. Many still default to prescribing individual meds because that’s what they learned in med school.
Also, pharmacy rules vary by state. In 42 states, pharmacists can swap a brand for a generic without asking. In 18, they need your permission. That means you might get a brand-name pill even if a cheaper generic combo exists-unless you speak up.
And insurance? Sometimes they make it harder. A plan might cover a brand-name combo because it’s "convenient," even if two generics cost half as much. Always check your formulary. Call your insurer. Ask: "Is there a generic combination that’s covered?"
What’s Next for Combination Generics?
The future is brighter.
The FDA released new draft guidelines in 2021 to speed up approval of fixed-dose cardiovascular combos. The World Heart Federation is pushing for polypills in low-income countries, where 80% of heart disease deaths occur. If widely adopted, these combos could prevent 15-20 million deaths globally in the next decade.
More combos are coming. Researchers are testing combinations with newer drugs like SGLT2 inhibitors (for heart failure and diabetes) and PCSK9 inhibitors. We’re not far from a single pill that covers blood pressure, cholesterol, blood sugar, and anti-clotting-all in one.
Right now, the biggest barrier isn’t science. It’s awareness. Patients don’t ask. Doctors don’t offer. Pharmacies don’t push.
But you can change that.
What Should You Do Today?
If you’re on multiple heart meds:
- Make a list of every pill you take, including dose and frequency.
- Ask your pharmacist: "Are there any combination generics I could switch to?" They know the latest options.
- Ask your doctor: "Is there a single pill that covers my needs?" Don’t accept "no" without a reason.
- Check your insurance formulary online. Look for "fixed-dose combination" or "combo" in the drug list.
- If you’re switched to a generic and feel different, tell your doctor. Don’t assume it’s "all in your head."
Heart disease doesn’t care if your pills are expensive or cheap. It only cares if you take them.
One pill instead of four. That’s the difference between staying healthy and ending up back in the hospital.
Are cardiovascular combination generics safe?
Yes, for most people. The FDA requires generic combination drugs to match brand-name drugs in strength, purity, and performance. Bioequivalence studies prove they deliver the same amount of active ingredient into your bloodstream. Over 60 clinical trials reviewed in the European Heart Journal found no meaningful safety differences between generics and brand-name cardiovascular drugs.
Why do some people say generics don’t work as well?
Some patients notice minor differences in side effects-like dizziness or fatigue-after switching. This is usually due to inactive ingredients (fillers, coatings) in the pill, not the active drug. For most, it’s harmless. But for those with narrow therapeutic windows-like on warfarin or with severe heart failure-doctors may recommend sticking with a brand or monitoring closely after a switch.
Can I switch from brand-name combo pills to generics on my own?
No. Always talk to your doctor first. Even though generics are safe, switching medications can affect your condition. Your doctor will check your blood pressure, kidney function, and electrolytes to make sure the switch is safe. Never stop or change your meds without medical advice.
What if my insurance won’t cover the generic combo?
Ask your doctor to file a prior authorization or appeal. Many insurers will cover the generic combo if you prove it’s cheaper and just as effective. You can also ask your pharmacist about patient assistance programs or discount cards-many generics cost under $10 with a GoodRx coupon.
Is there a "polypill" with aspirin, statin, beta-blocker, and ACE inhibitor in one pill?
Not yet in the U.S. While each of these drugs is available as a generic, no single pill combines all four. Some countries, like India and the UK, offer this for high-risk patients. In the U.S., you’ll need two or three pills. But research is ongoing, and such a pill may become available in the next few years.
How much money can I save with combination generics?
On average, generic combination pills cost 80-85% less than brand-name versions. For example, a brand-name combo might cost $85 per month, while the generic version runs $15-$20. That’s $800-$900 saved per year per person. Multiply that across millions of patients, and the savings reach billions.


Latrisha M. on 15 November 2025, AT 00:24 AM
My dad switched to a generic combo for blood pressure and cholesterol last year. He used to forget half his pills. Now he takes one in the morning and one at night. His BP is better, and he’s saving $70 a month. No more pillbox chaos.