Ever wonder why a seemingly "uterine" problem can make you feel down, irritable, or foggy? It’s not magic - it’s hormones, and when the lining of the uterus grows too thick, the hormonal balance can shift enough to affect brain chemistry. Below we break down what endometrial hyperplasia mood changes look like, why they happen, and what you can do about them.
Key Takeaways
- Endometrial hyperplasia is an over‑growth of the uterine lining usually driven by excess estrogen.
- Hormonal swings tied to the condition can lower serotonin and raise cortisol, leading to depression‑like symptoms.
- Typical mood signs include irritability, anxiety, brain‑fog, and disrupted sleep.
- Seek medical help if you notice heavy or irregular bleeding combined with persistent mood changes.
- Lifestyle tweaks (diet, stress management, targeted therapy) often improve both the lining and mood.
What Is Endometrial Hyperplasia?
Endometrial Hyperplasia is a condition where the inner lining of the uterus (the endometrium) grows thicker than normal. It usually occurs when estrogen levels stay high without enough progesterone to counterbalance them. Common triggers include obesity, polycystic ovary syndrome (PCOS), diabetes, and certain hormone‑replacement therapies.
While many cases are benign, the thickened lining can progress to abnormal bleeding and, in a minority of cases, to cancer. Because the endometrium is a hormone‑sensitive tissue, any disruption can ripple through the body’s neuro‑endocrine system.
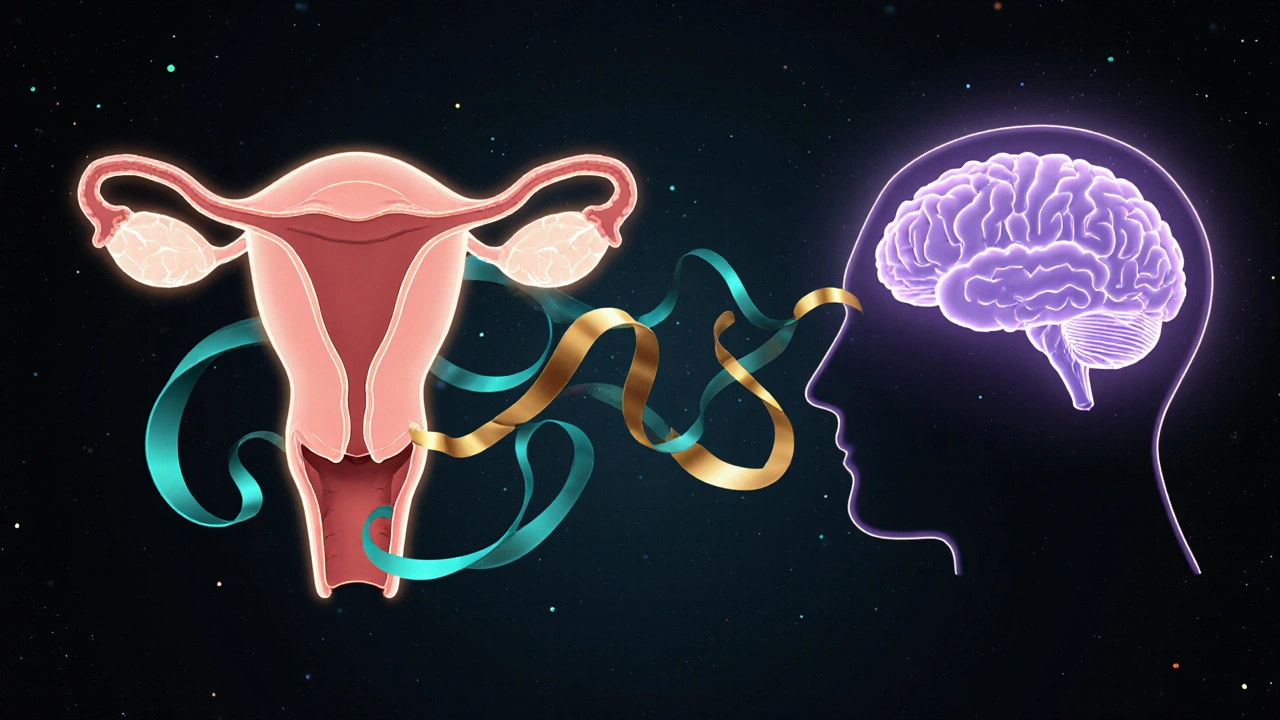
How Hormones Bridge the Uterus and the Brain
The brain talks to the uterus through the endocrine system. Two key players are Estrogen and progesterone. Estrogen boosts the growth of the endometrium, while progesterone stabilizes it.
When estrogen dominates, it also influences neurotransmitters. It can increase the activity of Serotonin, the 'feel‑good' chemical, but paradoxically, chronic high estrogen can lead to serotonin receptor down‑regulation, leaving you feeling flat or anxious.
At the same time, elevated estrogen raises Cortisol, the stress hormone. High cortisol scores long‑term fatigue, difficulty concentrating, and heightened irritability.
These hormonal swings explain why many women with endometrial hyperplasia report mood symptoms that mimic depression or anxiety, even if they have no prior mental‑health diagnosis.

Typical Mood Symptoms Linked to an Overgrown Lining
- Irritability: Small frustrations feel magnified.
- Low mood or sadness: A lingering sense of “blah” without a clear trigger.
- Heightened anxiety: Racing thoughts, restlessness, or feeling on edge.
- Brain fog: Trouble focusing, forgetfulness, or mental sluggishness.
- Sleep disturbances: Trouble falling asleep or waking up early.
These symptoms often appear alongside physical signs such as heavy or irregular periods, pelvic pressure, and spotting between cycles. The overlap can make it hard to pinpoint the cause, which is why a medical evaluation is essential.
When to Seek Medical Advice
- Bleeding that’s heavier than usual, lasts longer than 7‑10 days, or occurs at irregular intervals.
- Persistent mood changes (depression, anxiety, irritability) lasting more than two weeks and not improving with typical coping strategies.
- Pelvic pain, pressure, or a feeling of fullness in the lower abdomen.
- History of PCOS, obesity, or diabetes - risk factors that increase the likelihood of hyperplasia.
- Any new symptom that feels out of the ordinary for your normal menstrual cycle.
Doctors typically confirm the diagnosis with a transvaginal ultrasound and, if needed, an endometrial biopsy. Once confirmed, treatment focuses on rebalancing hormones and, if required, removing the excess tissue.
Treatment Options and Mood‑Friendly Strategies
Therapies aim to lower estrogen dominance and restore progesterone balance. Common approaches include:
- Progestin therapy: A daily pill or intrauterine device (IUD) that delivers progesterone directly to the uterus, thinning the lining and often improving mood.
- Weight management: Losing even 5‑10% of body weight can lower estrogen produced by fat tissue, easing both lining growth and emotional swings.
- Metformin (often used for PCOS): Helps improve insulin sensitivity, which indirectly reduces estrogen production.
- Lifestyle tweaks: Regular aerobic exercise, a Mediterranean‑style diet rich in omega‑3s, and stress‑reduction techniques (mindfulness, yoga) bolster serotonin and lower cortisol.
- Psychological support: Counseling or CBT can give you tools to manage anxiety and depressive feelings while the physical treatment takes effect.
Most women notice mood improvements within a few weeks of starting progestin therapy, especially when combined with lifestyle changes.
Quick Comparison: Normal Endometrium vs. Hyperplastic Lining
| Aspect | Normal Lining | Hyperplastic Lining |
|---|---|---|
| Thickness (mm) | 5‑12 (follicular phase) | >15, often 20‑30 |
| Hormonal balance | Estrogen ↔ Progesterone | Estrogen dominant, low progesterone |
| Bleeding pattern | Regular, predictable | Heavy, irregular, spotting |
| Mood impact | Stable | Irritability, anxiety, low mood |
| Risk of cancer | Very low | Increased (especially atypical hyperplasia) |
Practical Tips to Keep Mood Stable While Treating Hyperplasia
- Track your cycle and emotions: Use a simple notebook or app to note bleeding, pain, and mood each day. Patterns help your doctor adjust treatment.
- Prioritize sleep: Aim for 7‑9 hours; consistent bedtime reduces cortisol spikes.
- Eat for hormonal health: Include cruciferous veggies (broccoli, kale) that support estrogen metabolism. Limit processed sugars that fuel insulin spikes.
- Move daily: Even a 20‑minute walk releases endorphins, lifts serotonin, and helps weight control.
- Consider supplements wisely: Vitamin D and magnesium have been shown to improve mood and may aid hormonal balance. Consult your GP before adding anything.
- Stay connected: Talk to friends, join a women’s health forum, or see a therapist. Emotional support buffers stress.
Frequently Asked Questions
Can endometrial hyperplasia cause depression?
Yes. The hormonal imbalance-especially high estrogen with low progesterone-can lower serotonin and raise cortisol, which together manifest as depressive symptoms in many women.
Is mood change a sign that the hyperplasia is getting worse?
Worsening mood often mirrors worsening hormonal imbalance. If you notice your irritability or anxiety intensifying along with heavier bleeding, it’s worth re‑checking with your clinician.
Can a hormonal IUD improve my mood?
Many women experience mood stabilization after a levonorgestrel IUD is placed, because it delivers progesterone locally, thins the lining, and reduces systemic estrogen spikes.
Do lifestyle changes alone cure hyperplasia?
Lifestyle shifts-weight loss, balanced diet, regular exercise-can dramatically lower estrogen production and may reverse mild hyperplasia, but medical supervision is essential to rule out atypical cases that need medication.
Should I see a mental‑health professional if I feel down?
Absolutely. Addressing both the physical cause (hyperplasia) and the emotional impact together gives the best outcome. A therapist can provide coping tools while your doctor treats the uterine condition.



Macy Weaver on 13 October 2025, AT 21:23 PM
I’ve dealt with endometrial hyperplasia for a couple of years, and the mood swings really caught me off‑guard. The excess estrogen was literally making me feel on edge even on days when my period was light. Tracking both my cycle and my emotions in a simple notebook helped my doctor fine‑tune the progestin dose. Adding a daily walk and a few servings of leafy greens seemed to ease the brain‑fog a bit. If you’ve noticed similar irritability, try pairing medical treatment with a consistent sleep schedule – it’s a game‑changer.