Fentanyl Withdrawal Timeline Calculator
This tool estimates when withdrawal symptoms may begin based on your last patch removal time. Always consult your doctor for medical advice—this is not a substitute for professional care.
Withdrawal Timeline Results
Select your last patch removal time to see symptom progression.
Using a fentanyl patch might seem simple-stick it on your skin, and it delivers pain relief for three days. But behind that quiet, adhesive patch is a drug 50 to 100 times stronger than morphine. One wrong move-heat on the skin, a child finding a used patch, or stopping too fast-can turn a life-saving tool into a deadly threat. This isn’t hypothetical. Between 1997 and 2012, 32 children died after accidentally coming into contact with discarded fentanyl patches. And every year, hundreds of adults experience severe withdrawal or overdose because they didn’t understand how this medicine really works.
How Fentanyl Patches Work (And Why That’s Dangerous)
Fentanyl patches are designed for people with severe, long-term pain-like advanced cancer or chronic nerve damage-who need constant pain control and can’t rely on pills. Unlike oral painkillers that spike and drop in your bloodstream, the patch slowly releases fentanyl through your skin over 72 hours. That steady flow helps avoid the highs and crashes of pills. But that same feature makes it dangerous. The patch doesn’t start working right away. It takes 12 to 24 hours to reach full strength. If you’re new to opioids and put one on thinking it’ll give quick relief, you’re risking overdose before you even feel the pain fade. That’s why doctors only prescribe them to people already used to strong opioids-those taking at least 60 mg of morphine daily for a week or more. If you’ve never taken opioids before, this patch is not for you. And heat? That’s a silent killer. A hot bath, a heating pad, even a fever can make your skin absorb fentanyl faster. One study found body temperature rising just 2°C could double the amount of drug entering your blood. That’s enough to shut down breathing. The FDA issued warnings about this in 2013. Yet, people still use saunas or wear patches while getting a massage with warm oils. Don’t.Overdose: The Silent Emergency
An overdose from a fentanyl patch doesn’t look like a movie scene. There’s no screaming, no falling to the floor. It’s quiet. Too quiet. Symptoms include:- Slow, shallow, or stopped breathing
- Cold, clammy skin
- Blue lips or fingernails
- Unresponsiveness-no reaction to loud noises or shaking
- Pupils like pinpoints
- Extreme drowsiness or passing out
Withdrawal: When Stopping Becomes a Nightmare
Stopping fentanyl patches suddenly isn’t like quitting caffeine. It’s like pulling the plug on your nervous system after months of constant stimulation. Withdrawal symptoms start 8 to 24 hours after your last patch. They peak at 36 to 72 hours and can last 7 to 10 days-or longer if you’ve been on a high dose for months. Symptoms include:- Severe anxiety and agitation
- Insomnia, nightmares
- Sweating, chills, goosebumps
- Runny nose, watery eyes
- Yawning nonstop
- Stomach cramps, vomiting, diarrhea
- Fast heartbeat, high blood pressure
- Muscle aches, bone pain
- Depression, suicidal thoughts

What You Must Do to Stay Safe
If you’re prescribed a fentanyl patch, here’s what you need to do:- Never use heat. No hot tubs, saunas, heating pads, or sunbathing with the patch on.
- Keep patches locked up. Even used ones. Children and pets don’t know the difference.
- Dispose of patches properly. Fold sticky side to sticky side. Flush? Only if your doctor says so. Most places recommend mixing with coffee grounds or cat litter before throwing in the trash.
- Carry naloxone. If your doctor doesn’t offer it, ask. It’s life-saving.
- Tell every doctor and dentist you see. Even for a tooth extraction or surgery. Fentanyl interacts dangerously with anesthesia and other sedatives.
- Never share your patches. Not even with a family member who has pain. This isn’t a painkiller-it’s a controlled substance with a high risk of death.
- Don’t stop without talking to your doctor. If you want to quit, make a plan. Tapering is not optional.
Alternatives and When to Ask for Help
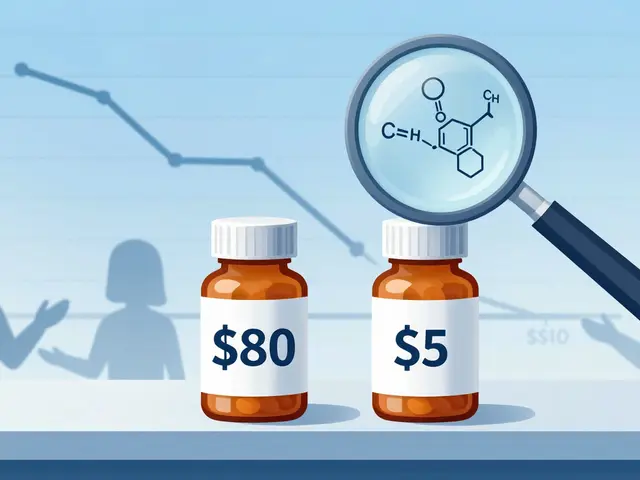
Fentanyl patches aren’t the only option for chronic pain. Physical therapy, nerve blocks, antidepressants for nerve pain, acupuncture, and even mindfulness-based pain management have helped many people reduce or eliminate opioid use. The CDC now recommends trying non-opioid treatments first. If you’re struggling with your patch-feeling too sleepy, having trouble breathing, or dreading withdrawal-talk to your doctor. If you feel trapped, or think you might be developing a dependence, reach out to a pain specialist or addiction counselor. You’re not weak for needing help. You’re smart for asking. The number of fentanyl patch prescriptions in the U.S. dropped 42% between 2016 and 2022. Why? Because doctors and patients are learning the truth: this drug saves lives when used right, but it can end them just as easily when used wrong.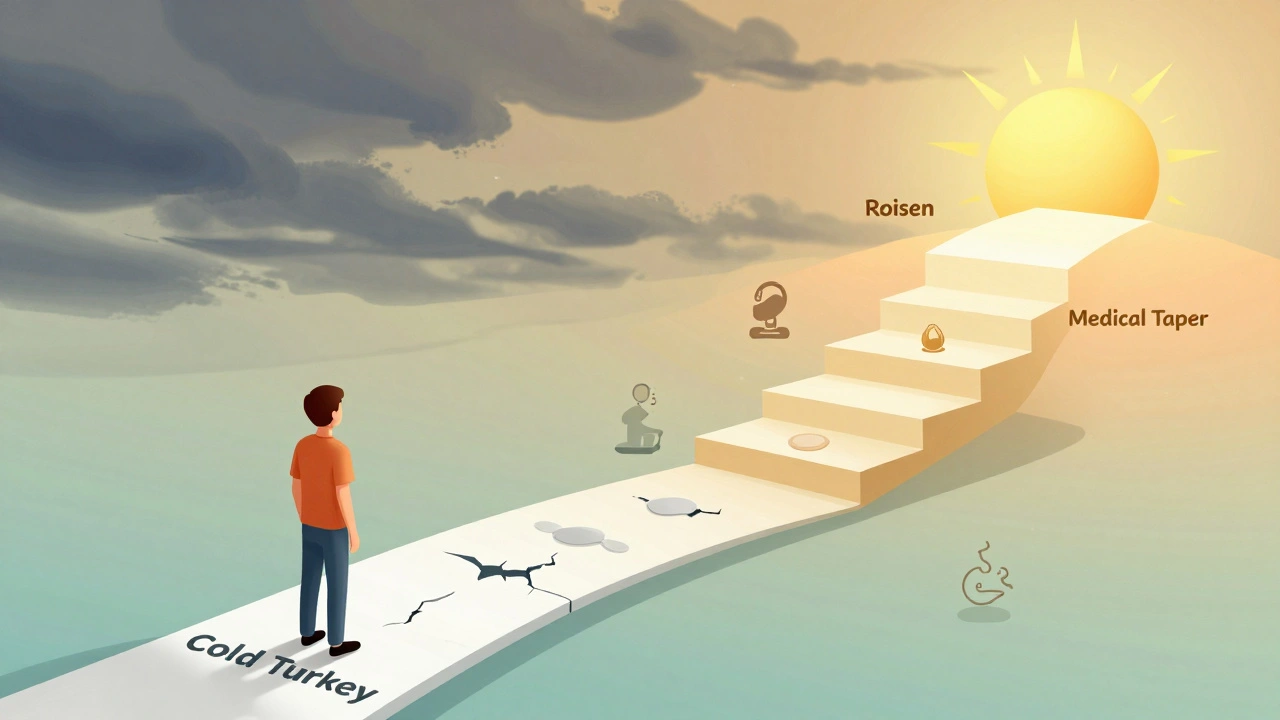
Frequently Asked Questions
Can you die from fentanyl patch withdrawal?
Withdrawal from fentanyl patches is not usually life-threatening like alcohol or benzodiazepine withdrawal. But it can lead to serious complications. Severe vomiting and diarrhea can cause dehydration, which raises sodium levels in your blood and may trigger heart rhythm problems. In rare cases, this can lead to heart failure. That’s why medical supervision during tapering is strongly recommended.
How long does a fentanyl patch stay in your system?
The patch delivers fentanyl for 72 hours, but the drug can stay detectable in your body for up to 7 days after removal. It’s stored in fat tissue and slowly released. That’s why withdrawal symptoms can linger longer than expected. Drug tests can detect fentanyl in urine for 24 to 72 hours after the last patch, and in hair for up to 90 days.
Can you cut a fentanyl patch to lower the dose?
Never cut, chew, or alter a fentanyl patch. The drug is stored in a gel reservoir, and cutting it can cause the entire dose to leak out at once. This has caused fatal overdoses. If you need a lower dose, your doctor will prescribe a different strength. Never adjust it yourself.
Is it safe to use fentanyl patches with alcohol?
No. Alcohol, even one drink, can increase the risk of overdose by slowing your breathing even more. The FDA warns that combining fentanyl with alcohol can cause respiratory failure and death. Avoid all alcohol while using this patch.
What should I do if I miss a patch change?
If you miss changing your patch by less than 12 hours, apply the new one as soon as you remember. If you’re more than 12 hours late, skip the missed dose and apply the next patch at your regular time. Don’t double up. Missing doses can trigger withdrawal. Taking extra patches increases overdose risk. Always stick to your schedule.



Kenny Leow on 2 December 2025, AT 01:12 AM
Been using these patches for chronic neuropathy for 5 years. The heat warning saved my life-once I skipped my sauna routine after reading this, my bloodwork went from scary to stable. Seriously, if you're on this, treat it like a live grenade with a timer.