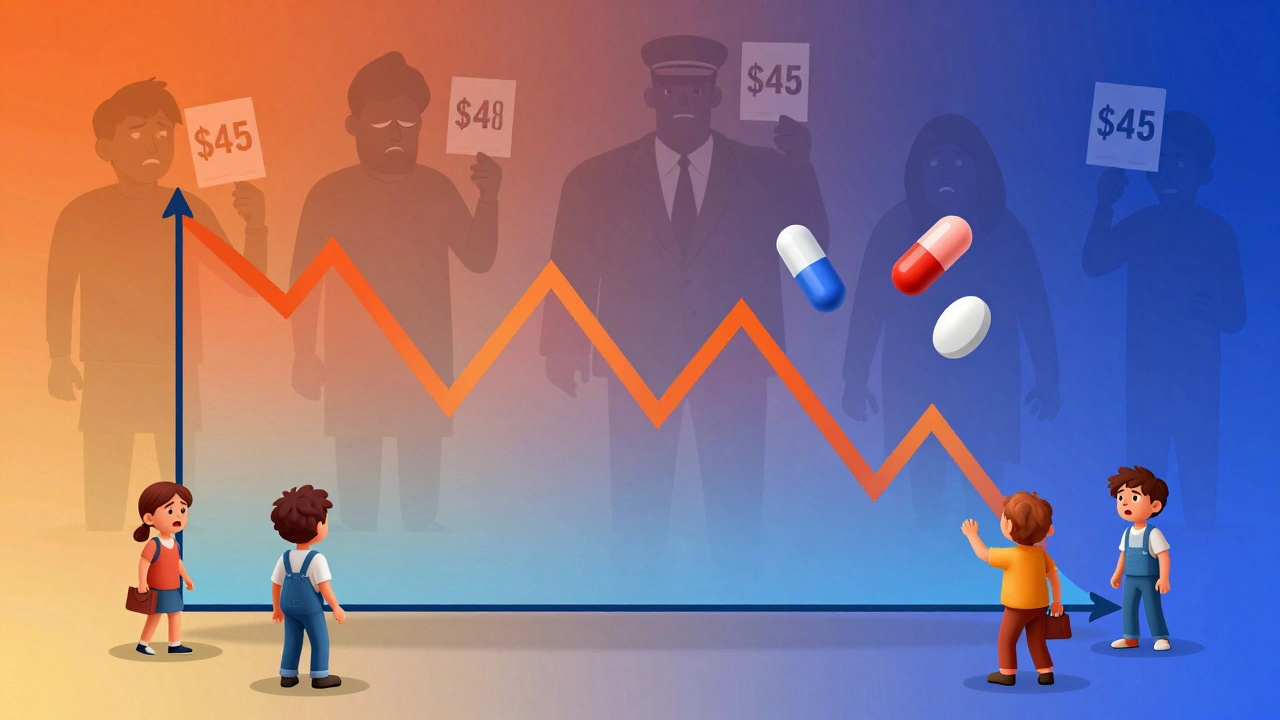
For most people, generic drugs are the reason they can afford their prescriptions. They’re the same medicine as the brand-name version, just cheaper. But here’s the problem: generic drug prices don’t always stay cheap. Some drop sharply. Others spike overnight - sometimes by hundreds of percent. If you’ve seen your $4 pill jump to $45 in a year, you’re not imagining it. This isn’t rare. It’s the new reality of how generics work.
How Generic Drug Prices Usually Drop - and Why They Sometimes Don’t
When a brand-name drug’s patent expires, the FDA starts approving copies. The first generic maker usually sets a price around 90% of the brand’s cost. That’s already a big discount. But once a second company enters, prices drop to about 65%. With a third, they fall to 52%. By the time four or more companies are selling the same drug, prices can be as low as 15% of the original brand price.
This is how it’s supposed to work. More competition = lower prices. And for many drugs, that’s exactly what happens. Take levothyroxine, the thyroid medication. Between 2013 and 2018, its price dropped 87% because dozens of companies made it.
But not all drugs follow this pattern. If only one or two companies make a generic, prices don’t fall. They can even go up. In fact, 78% of generic price hikes over 100% happened in markets with three or fewer manufacturers. That’s not an accident. It’s a structural flaw in the system.
Year-by-Year Price Swings: The Real Numbers
Looking at the big picture, generic drug prices have gone down overall since 2008. The U.S. saved $2.2 trillion on generics between 2008 and 2017. That’s huge. But averages hide the chaos.
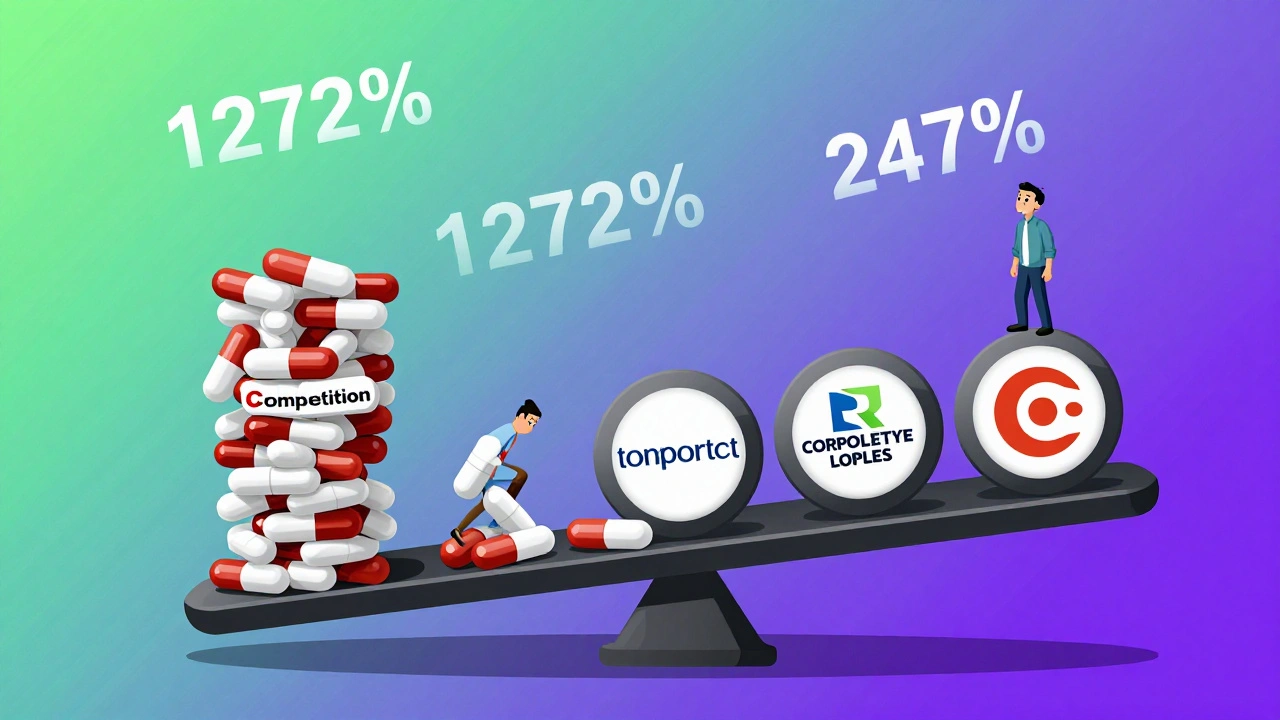
In 2023, the overall list price for generics rose just 4.9% - a small number. But that number doesn’t tell the whole story. Between January 2022 and January 2023, about 40 generic drugs saw price increases averaging 39%. One of them, nitrofurantoin macrocrystals, jumped 1,272% over five years.
Medicaid data from 2013-2014 showed that 8.2% of generic prescriptions had price surges between 100% and 500%. And those weren’t outliers. They were symptoms. The same thing happened again in 2022-2023. GoodRx data shows lisinopril, a common blood pressure pill, went from $4 to $45 at Walmart in just 18 months - a 247% increase.
Here’s the breakdown of what happens to generic prices each year:
- 60% of generics: stable (change under 5%)
- 25% of generics: moderate fluctuation (5-20%)
- 15% of generics: major swings (over 20%)
That last group - just 15% of drugs - accounts for 60% of all spending growth in the generic market. That means a tiny number of drugs are driving up costs for everyone.
Why Do Some Generic Drugs Spike in Price?
It’s not about manufacturing costs. It’s about control.
Between 2013 and 2018, the number of companies making generic drugs dropped from 150 to 80. Today, the top 10 manufacturers control 70% of the market. The top five hold 52% - up from 38% in 2015. That’s consolidation. And when only a few players are left, they can raise prices without fear of losing customers.
Supply chain problems make it worse. In 2023, the FDA found quality issues at 23% of foreign generic manufacturing plants. When one factory gets shut down, the supply of that drug shrinks. If only one other company can make it, prices jump. That’s what happened with generic doxycycline, a common antibiotic. When one big manufacturer left the market, the price doubled overnight.
There’s also the Medicaid Best Price rule. It forces manufacturers to offer the same low price to Medicaid as they do to anyone else. That means they can’t undercut each other easily. So instead of competing on price, they compete on who can stay in business the longest - and sometimes, that means raising prices when they can.

Who Gets Hit the Hardest?
It’s not just patients. Pharmacies are caught in the middle.
Independent pharmacies report that 42% of them saw profit margins collapse on 15% of their generic drugs. One week, a drug is profitable. The next, it’s a loss leader. Some pharmacies have to absorb price hikes of $3.75 per prescription just to keep stocking the medicine.
Patients are feeling it too. A 2024 KFF survey found that 37% of Medicare beneficiaries taking generics skipped doses because they couldn’t afford them. That’s nearly four in ten seniors choosing between medicine and groceries.
And it’s not just low-income people. Even those with insurance aren’t safe. Many plans have high copays for certain generics. If the price spikes, your $10 copay can turn into $50 - even if your insurance covers 80%.
What’s Changing Now?
There’s some hope. The Inflation Reduction Act didn’t directly cap generic prices, but it changed how rebates work. In January 2024, over 20 brand-name drugs dropped prices because of new Medicaid rules - though generics didn’t react as much.
The FDA is trying to fix the problem. Their 2024 plan targets faster approvals for generics with few competitors. They want to cut review times by 20% for these drugs. That means more companies could enter the market faster - and bring prices down.
The FTC is also stepping in. As of June 2024, they had 12 active investigations into unjustified price hikes in generic markets with limited competition. These aren’t random audits. They’re focused on companies that raised prices 100% or more when only one or two others made the same drug.
Long-term, experts predict generic prices will grow at just 1.5% per year through 2030 - far slower than brand-name drugs. But that’s an average. The real risk is still in the 15% of drugs with high vulnerability - especially heart and brain medications like statins, antidepressants, and seizure drugs.
What You Can Do Right Now
Don’t just accept the price on the receipt. Here’s what works:
- Check GoodRx or SingleCare before you pay. You’ll often find prices 50% lower than the pharmacy’s cash rate.
- Ask your pharmacist if there’s a different manufacturer. Sometimes, switching brands within the same generic lowers the cost.
- Call your insurance. Ask if they have a preferred generic - sometimes they do.
- If your drug spiked in price, ask your doctor about alternatives. Not all generics are equal in cost.
- Use mail-order pharmacies. They often have better pricing on maintenance medications.
And if you’re paying over $100 a month for a generic that used to cost $20 - you’re not alone. Report it. Contact your state’s attorney general. File a complaint with the FTC. These price spikes aren’t inevitable. They’re the result of market failures. And they can be fixed - if enough people speak up.
Why are generic drug prices so unpredictable?
Generic drug prices are unpredictable because they depend on competition. When many companies make the same drug, prices drop. But if only one or two manufacturers are left, they can raise prices without losing customers. Supply chain issues, factory shutdowns, and market consolidation make this even worse. A drug that costs $5 one year can jump to $50 the next if the only other maker exits the market.
Are generic drugs always cheaper than brand-name drugs?
Yes, but not always by much. Most generics cost 80-85% less than the brand version. But in markets with little competition, some generics can cost nearly as much as the original brand. For example, a generic version of a heart drug might still cost $200 a month if only one company makes it. That’s why checking prices with tools like GoodRx is essential.
Which generic drugs are most likely to spike in price?
Drugs with few manufacturers are the biggest risk. Cardiovascular medications like warfarin and generic statins, central nervous system drugs like levetiracetam and gabapentin, and older antibiotics like doxycycline are common culprits. These are often high-volume drugs with low profit margins - so when manufacturers leave the market, the rest can raise prices sharply.
Can I switch to a different generic version of my drug?
Yes, and you should. Generic drugs contain the same active ingredient, so switching manufacturers won’t change how the drug works. But the price can be very different. Ask your pharmacist which generic version your pharmacy carries and what each one costs. Sometimes, one brand of generic is half the price of another.
Why do pharmacy prices for the same generic vary so much?
Pharmacies buy drugs at different prices based on contracts with distributors. Some get better deals than others. Also, pharmacies set their own cash prices - not based on what they paid, but on what they think patients will pay. That’s why GoodRx often shows prices lower than the pharmacy’s listed price. The pharmacy may be charging more because they know you don’t have insurance or won’t shop around.
Is there a way to lock in a low price for my generic medication?
You can’t lock in a price permanently, but you can reduce risk. Use mail-order pharmacies for maintenance meds - they often offer 90-day supplies at lower rates. Some retailers like Costco or Walmart have $4 lists for common generics. And if your drug is on a price spike, ask your doctor for a 3-month supply at the current price before it jumps again. You can also apply for patient assistance programs through drug manufacturers.
What’s Next for Generic Drug Prices?
The system isn’t broken - it’s just unbalanced. Generics saved the U.S. healthcare system over $2 trillion in the last decade. But that success created a new problem: too much consolidation, too little competition, and too many vulnerable markets.
Regulators are waking up. The FDA, FTC, and CMS are all taking steps to increase competition and punish price gouging. But change moves slowly. In the meantime, patients and pharmacies are left to navigate a minefield of unpredictable costs.
The lesson is simple: don’t assume your generic will stay cheap. Always check. Always compare. And never be afraid to ask why a price changed. Your health - and your wallet - depend on it.



Fern Marder on 3 December 2025, AT 05:05 AM
OMG this is wild 😱 I just paid $52 for my generic blood pressure med last week-last year it was $8. My pharmacist shrugged and said, 'Welcome to 2024.'