Cholesterol Medication Selector
If you’ve been told to lower your LDL cholesterol, you’ve probably heard the name Lipitor - the brand name for atorvastatin, a statin that blocks the HMG‑CoA reductase enzyme to cut cholesterol production. While Lipitor remains a go‑to option, an ever‑growing list of alternatives means the “one‑size‑fits‑all” answer rarely works. This guide walks you through the key factors that matter, compares the most common substitutes, and helps you figure out which pill matches your health profile and lifestyle.
Key Takeaways
- Lipitor is a high‑intensity statin with strong LDL‑lowering power but can cause muscle aches and interact with certain meds.
- Crestor (rosuvastatin) offers similar potency with a slightly lower risk of drug interactions.
- Older statins like Zocor (simvastatin) and Mevacor (lovastatin) are cheaper but less potent and may need higher doses.
- Non‑statin options-Zetia (ezetimibe) and PCSK9 inhibitors (alirocumab, evolocumab)-are useful when statins are not tolerated.
- Choosing the right drug depends on LDL target, existing health conditions, cost, and how your body reacts.
How Lipitor Works and Who It Helps
Atorvastatin belongs to the statin class, which reduces cholesterol by inhibiting the liver enzyme HMG‑CoA reductase. The result is a 30‑55% drop in LDL for most users, making it a high‑intensity choice for people with:
- Existing heart disease or a history of heart attacks.
- Diabetes combined with elevated LDL.
- Very high baseline cholesterol (>190 mg/dL).
Typical dosing starts at 10mg daily, with a ceiling of 80mg for those needing aggressive reductions. Side effects can include muscle pain, elevated liver enzymes, and, rarely, memory issues. Because atorvastatin is metabolized by the CYP3A4 pathway, drugs like certain antifungals, antibiotics, and grapefruit juice can boost its level and raise side‑effect risk.

Decision Criteria: What to Compare
When weighing Lipitor against other options, look at these five pillars:
- Efficacy - how much LDL does the drug cut at standard doses?
- Safety profile - frequency of muscle symptoms, liver impacts, and drug‑drug interactions.
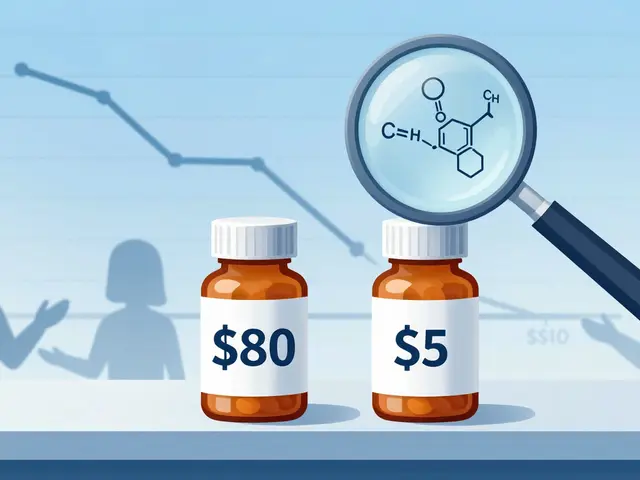
- Cost & insurance coverage - generic availability and out‑of‑pocket expense.
- Dosing convenience - once‑daily pill versus injectable or multiple‑dose regimens.
- Special population fit - renal or hepatic impairment, pregnancy, or genetic lipid disorders.
Below you’ll see how the most common alternatives stack up against Lipitor across these criteria.
Comparison Table: Lipitor vs Popular Alternatives
| Drug (Brand) | Generic Name | Typical LDL Reduction | Key Side‑Effects | Cost (AU$ per month) | Metabolism Pathway |
|---|---|---|---|---|---|
| Lipitor | Atorvastatin | 30‑55% | Myalgia, ↑LFTs, rare rhabdomyolysis | ~20 (generic) | CYP3A4 |
| Crestor | Rosuvastatin | 35‑55% | Myalgia, ↑LFTs, mild diarrhea | ~25 (generic) | CYP2C9 (minor CYP3A4) |
| Zocor | Simvastatin | 20‑45% | Myalgia, ↑LFTs, increased diabetes risk | ~12 (generic) | CYP3A4 |
| Pravachol | Pravastatin | 20‑30% | Low muscle risk, mild GI upset | ~15 (generic) | Renal excretion (minimal CYP) |
| Mevacor | Lovastatin | 20‑35% | Myalgia, drug interactions (CYP3A4) | ~10 (generic) | CYP3A4 |
| Zetia | Ezetimibe | 15‑20% (as monotherapy) | Diarrhea, rare liver changes | ~30 (brand) | Minimal metabolism |
| Repatha | Evolocumab | 60‑70% (injectable) | Injection site reaction, nasopharyngitis | ~400 (specialist) | Monoclonal antibody |
Deep Dive into Each Alternative
Crestor (Rosuvastatin)
Crestor delivers LDL drops that rival Lipitor while having a lower reliance on CYP3A4, which means fewer interactions with common antibiotics or antifungals. It’s often the first switch for patients who experience muscle pain on atorvastatin. Dosage ranges from 5mg to 40mg daily. The main caution is a slightly higher risk of new‑onset diabetes at high doses.
Zocor (Simvastatin)
Zocor is an older, lower‑cost statin. It works well for moderate‑risk patients but should never exceed 20mg daily in patients taking certain antibiotics (e.g., clarithromycin) because of a spike in rhabdomyolysis cases. Its LDL‑lowering power tops out around 45%.
Pravachol (Pravastatin)
Pravachol is kidney‑excreted and avoids the CYP450 system entirely, making it a safe bet for patients on multiple meds. The trade‑off is modest LDL reduction (≈25%). It’s popular for older adults who can’t tolerate higher‑intensity statins.
Mevacor (Lovastatin)
Mevacor was the first statin on the market. It’s cheap and effective for those with mild hypercholesterolemia. Like Zocor, it’s metabolized by CYP3A4, so drug interactions are a concern. Typical doses are 20‑80mg daily.
Zetia (Ezetimibe)
Zetia blocks cholesterol absorption in the intestines. On its own it only trims LDL by about 15‑20%, but combined with a low‑dose statin it can achieve reductions comparable to high‑intensity statins, and it’s well‑tolerated. It’s a favorite when patients develop statin‑related muscle pain.
PCSK9 Inhibitors (Evolocumab, Alirocumab)
These injectable antibodies-marketed as Repatha (evolocumab) and Praluent (alirocumab)-cut LDL by 60‑70% even in people who can’t use statins. They’re pricey and usually reserved for familial hypercholesterolemia or patients with recurrent cardiovascular events despite maximal statin therapy.
Which Drug Fits Which Scenario?
Below is a quick match‑up. Consider your doctor’s advice, your insurance, and any personal concerns.
- High‑intensity needs (LDL > 190 mg/dL or recent heart attack): Lipitor 40‑80mg or Crestor 20‑40mg.
- Statin‑intolerant due to muscle pain: Switch to Pravachol or add Zetia.
- Multiple drug interactions (e.g., on HIV meds, certain antibiotics): Choose Crestor (less CYP3A4) or Pravachol (no CYP metabolism).
- Budget‑focused, moderate risk: Zocor or Mevacor generic versions.
- Genetic hypercholesterolemia or failed statin therapy: PCSK9 inhibitor injection.
Talking to Your Doctor: Practical Tips
- Bring a list of all current prescription, OTC, and herbal products.
- Ask about baseline liver enzymes and CK (creatine kinase) before starting.
- Clarify how often you’ll need blood‑test follow‑ups.
- Discuss cost‑sharing options; many insurance plans have lower co‑pays for generics.
- If you notice unexplained muscle soreness, report it immediately-dose adjustments can prevent serious harm.
Frequently Asked Questions
Can I switch from Lipitor to another statin without a wash‑out period?
Yes. Because most statins share the same mechanism, doctors usually transition you on the same day or after a short 2‑day gap. Your physician will monitor liver enzymes after the switch.
Is it safe to take Lipitor with grapefruit juice?
No. Grapefruit inhibits CYP3A4, raising atorvastatin levels and increasing the risk of muscle toxicity. Stick to non‑citrus juices if you’re on Lipitor.
How long does it take to see LDL reduction after starting Lipitor?
Most patients see a measurable drop within 2‑4 weeks, with the full effect appearing around 6‑8 weeks. Your doctor will repeat a lipid panel after that period.
Are PCSK9 inhibitors covered by Medicare in Australia?
They are listed on the Pharmaceutical Benefits Scheme (PBS) for very high‑risk patients, but eligibility requires documented statin intolerance or recurrent cardiovascular events.
What lifestyle changes boost the effectiveness of any cholesterol drug?
Adopt a Mediterranean‑style diet, aim for at least 150minutes of moderate exercise weekly, quit smoking, and keep weight within a healthy range. These steps can add an extra 10‑15% LDL reduction on top of medication.


Benjamin Cook on 10 October 2025, AT 09:06 AM
Hey folks!!! If you’re freaking out about cholesterol meds, don’t worry – we’ve got you covered!!! Lipitor rocks for high‑intensity needs, but remember those muscle aches if you overdo it – you might feel a bit sore, especially if you’re also taking antibiotics!!! And yes, grapefruit is a big NO‑NO!!! Keep an eye on your liver tests, and chat with your doc about dosing – they’ll help you find the sweet spot!!!