Most people with fatty liver don’t feel sick. No pain. No jaundice. No obvious warning signs. That’s why NAFLD sneaks up on so many-especially in places like Perth, where obesity and type 2 diabetes are rising fast. By the time symptoms show up, the damage might already be serious. The real question isn’t just whether you have fat in your liver-it’s whether that fat has turned dangerous.
What’s the difference between NAFL and NASH?
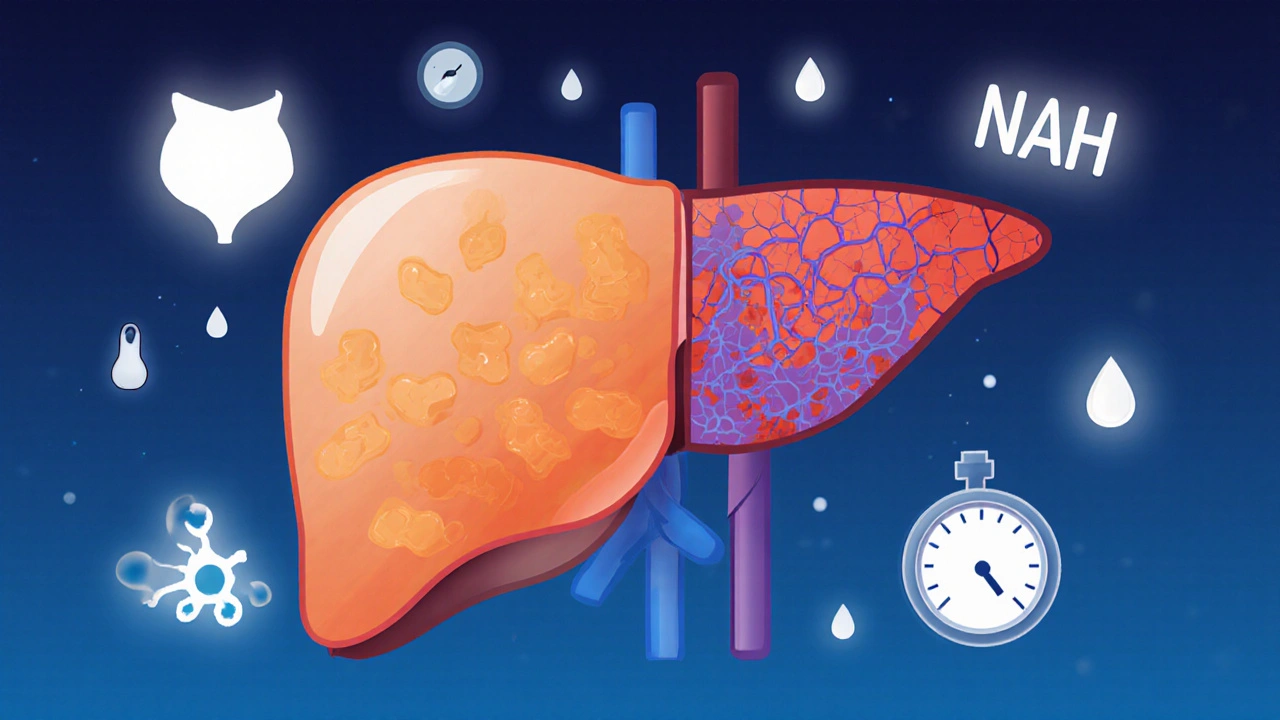
NAFLD stands for Non-Alcoholic Fatty Liver Disease. It’s not one condition. It’s a spectrum. At the mild end is NAFL-simple fatty liver. That means 5% or more of your liver is filled with fat, but there’s no inflammation, no cell damage, and no scarring. Most people with NAFL never progress. Their liver stays stable for years, even decades.
At the other end is NASH-Non-Alcoholic Steatohepatitis. This is the dangerous version. Same fat buildup-but now your liver cells are inflamed. They’re ballooning. Dying. And your body tries to repair the damage by laying down scar tissue. That’s fibrosis. And once fibrosis starts, it doesn’t always stop.
The shift from NAFL to NASH happens in about 1 in 5 people over 10-15 years. But not everyone who has fat in their liver will get NASH. Risk factors stack up: being overweight (especially with belly fat), having type 2 diabetes, high blood pressure, or high triglycerides. If you have three or more of these, you’re in the high-risk group.
Fibrosis is the real threat-not just the fat
Doctors used to focus on fat. Now they focus on fibrosis. Why? Because fibrosis predicts outcomes better than anything else.
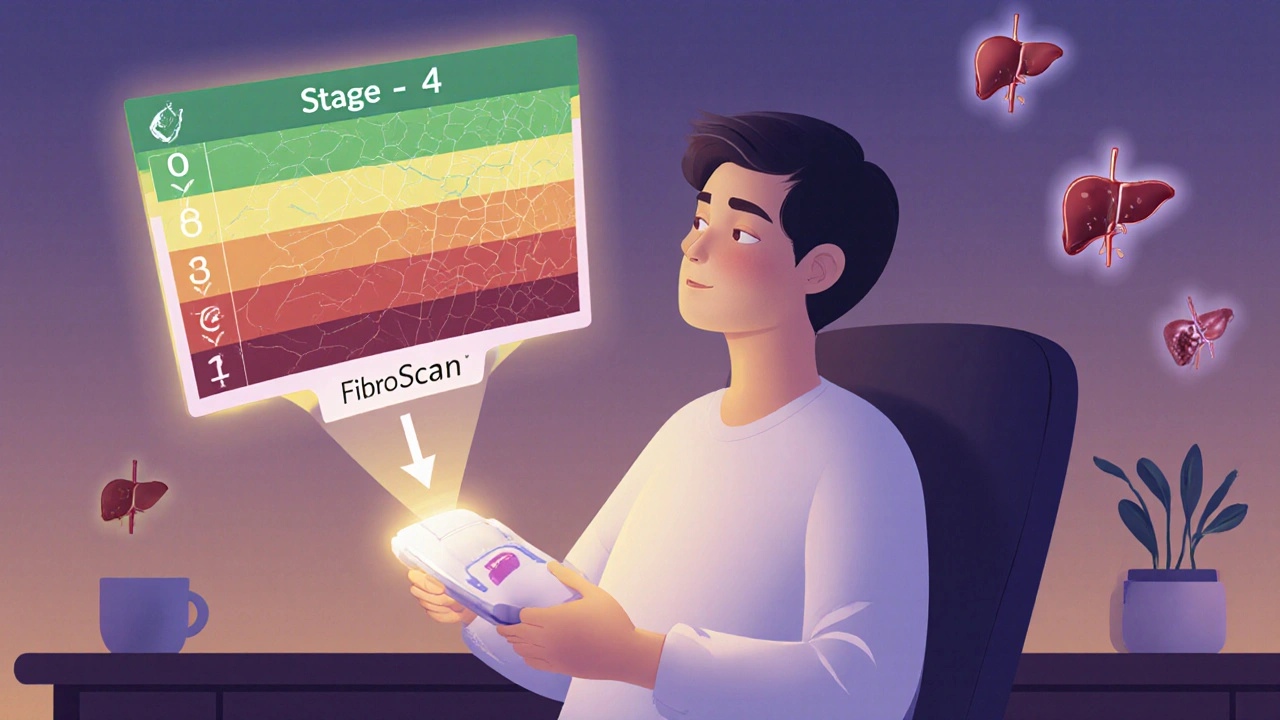
Fibrosis is scored from 0 to 4:
- Stage 0: No scarring
- Stage 1: Mild scarring around blood vessels
- Stage 2: Scarring spreading into liver tissue
- Stage 3: Bridging fibrosis-scars start connecting
- Stage 4: Cirrhosis-liver is permanently scarred, shrunken, and struggling
People with stage 3 or 4 fibrosis have a 12-25% chance of dying from liver disease within 10 years. Those with stage 0-2? Less than 2%. That’s a huge gap. And here’s the kicker: you can have NASH without advanced fibrosis-or you can have fibrosis without full-blown NASH. The fibrosis stage matters more than the NASH label.
A 2022 study tracking 1,245 patients over 15 years found that 41.7% of NASH patients developed advanced fibrosis. Only 12.3% of NAFL patients did. That’s more than triple the risk.
How do you know if you have NASH or just NAFL?
There’s no blood test that confirms NASH. No scan that shows inflammation for sure. The only way to be certain is a liver biopsy. But here’s the problem: most doctors won’t recommend one unless they strongly suspect advanced disease.
Instead, they use a mix of tools:
- ALT and AST blood tests: These liver enzymes rise when liver cells are damaged. Normal ALT is 7-55 U/L. If yours is consistently above 40 and you’re overweight? Red flag.
- FIB-4 score: Uses your age, ALT, AST, and platelet count. A score above 1.30 suggests possible fibrosis. Above 2.67? High risk for advanced scarring.
- FibroScan: A quick, painless ultrasound that measures liver stiffness. A reading over 7.1 kPa means significant fibrosis. Over 10 kPa? Likely stage 3 or 4.
- MRI-PDFF: The most accurate way to measure liver fat-up to 95% accurate. Not widely available, but growing.
Ultrasound can detect fat, but it misses mild cases. Blood tests can be normal even with NASH. That’s why so many people are diagnosed late. One Reddit user shared: "My ALT was 68 for three years. No symptoms. Then I got diagnosed with stage 2 fibrosis."
Who should be screened-and when?
You don’t need a scan if you’re healthy and lean. But if you have metabolic syndrome-three or more of these-you should get checked:
- Belly fat (waist over 40 inches for men, 35 for women)
- Triglycerides over 150 mg/dL
- HDL (good cholesterol) under 40 (men) or 50 (women)
- Blood pressure over 130/85
- Fasting blood sugar over 100 mg/dL
That’s about 1 in 3 adults in the U.S. and similar numbers in Australia. The American Association of Family Physicians recommends screening these people with a simple ALT test. If it’s high, next step: FibroScan or FIB-4.
Primary care doctors are getting better at this-but only 32% feel confident managing advanced cases. Wait times to see a liver specialist can be 90 days or more. That’s why early detection matters.
What happens if you do nothing?
NAFL? Probably nothing. You might live a normal life. NASH? That’s where things get risky.
- 20-40% of NASH patients develop cirrhosis in 10-20 years
- 5-12% develop liver cancer (hepatocellular carcinoma)
- 1.5-2 times higher risk of death than NAFL patients
And here’s the twist: the leading cause of death in NAFLD patients isn’t liver disease. It’s heart disease. Over 40% of deaths are from heart attacks or strokes. That’s because NAFLD and NASH aren’t just liver problems-they’re signs of metabolic chaos. Fat in the liver means fat in the arteries, too.
Can you reverse it?
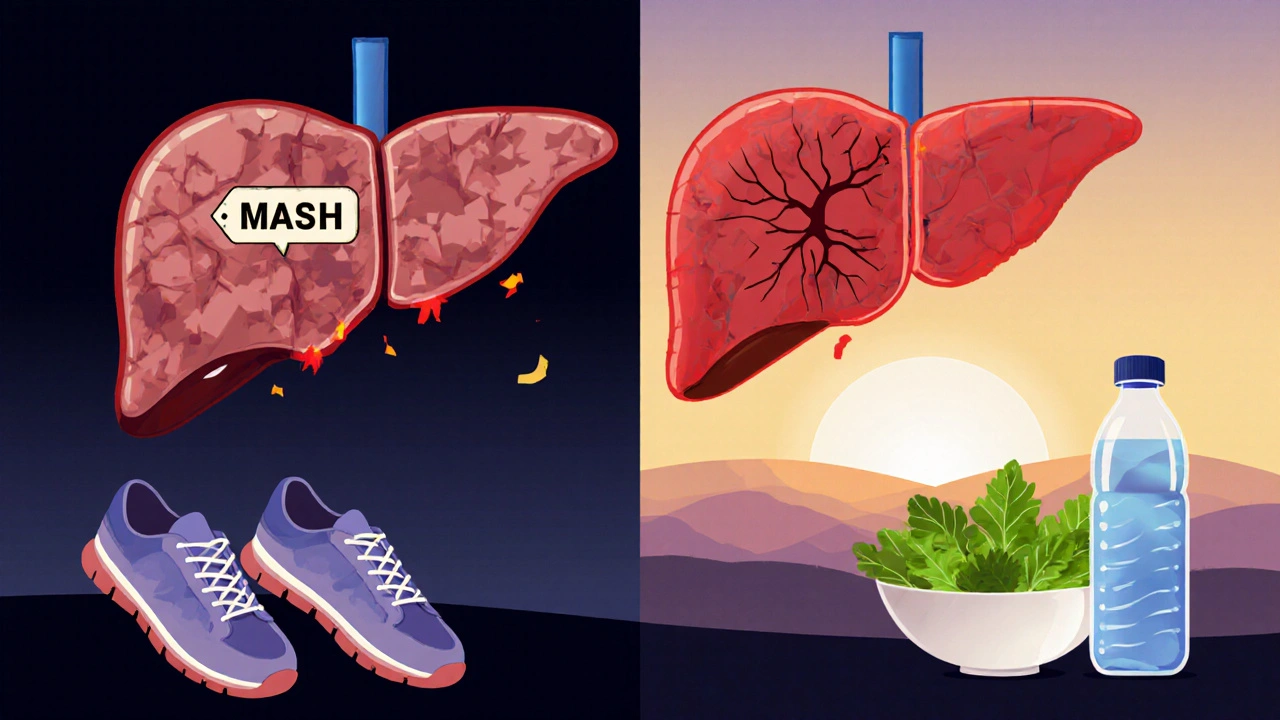
Yes. But only if you act early.
Weight loss is the most proven treatment. Losing 5-7% of your body weight can reduce liver fat. Lose 10%? You can reverse NASH and even improve fibrosis. One patient on a support forum wrote: "Lost 10% body weight in 18 months. My biopsy showed NASH turned back to simple fatty liver. No meds. Just diet and walking."
Exercise helps-even without weight loss. Just 150 minutes a week of brisk walking cuts liver fat and inflammation.
There’s no FDA-approved drug for NASH… yet. But in March 2023, the FDA approved resmetirom (Rezdiffra) for patients with moderate to advanced fibrosis. It’s the first drug shown to reduce liver fat and fibrosis. Still, it’s not a magic pill. You still need to lose weight. Still need to control diabetes. Still need to move.
The big shift: NAFLD and NASH are now called MASLD and MASH
In June 2023, liver experts around the world agreed to drop the "non-alcoholic" label. Why? Because it’s misleading. It sounds like you’re being blamed for drinking. But the real problem isn’t alcohol-it’s metabolism.
Now it’s:
- MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) - replaces NAFLD
- MASH (Metabolic Dysfunction-Associated Steatohepatitis) - replaces NASH
The new definition requires at least one metabolic risk factor: obesity, diabetes, high blood pressure, or abnormal cholesterol. This change helps doctors focus on the root cause: metabolic health.
By 2030, experts predict over one-third of the global population will have MASLD. Liver transplants for MASH could jump from 10% to 25% of all transplants in the U.S.
What should you do now?
If you’re overweight, diabetic, or have high blood pressure-get your liver checked. Don’t wait for symptoms. They rarely come until it’s too late.
Start with a basic blood test: ALT, AST, platelets. Ask for a FIB-4 calculation. If it’s above 1.3, push for a FibroScan. If you’re over 40 and have metabolic syndrome, don’t brush off "fatty liver" as harmless.
And if you’re told you have NAFL or NASH? Don’t panic. But don’t ignore it. Your liver can heal. But only if you act now. Lose weight. Move more. Control your blood sugar. Cut out sugary drinks. These aren’t "lifestyle changes"-they’re your treatment plan.
The good news? If you catch it early, you can reverse it. The bad news? Most people don’t find out until it’s too late. You don’t need a miracle drug. You just need to start.
Can you have fatty liver without being overweight?
Yes. While obesity is the biggest risk factor, about 10-15% of people with NAFLD are normal weight. This is called "lean NAFLD." It’s often linked to insulin resistance, genetics, or rapid weight loss. Even thin people with high triglycerides or type 2 diabetes can develop fatty liver.
Is alcohol allowed if you have NAFLD or NASH?
Doctors recommend avoiding alcohol completely. Even small amounts can worsen liver inflammation and fibrosis. The "non-alcoholic" label means alcohol isn’t the cause-but it can make things much worse. If you have NASH, alcohol increases your risk of cirrhosis and liver cancer.
Do supplements like vitamin E or milk thistle help?
Vitamin E (800 IU/day) is sometimes used in non-diabetic NASH patients under medical supervision-it’s shown modest benefit in reducing inflammation. But it’s not a cure and can have side effects. Milk thistle has no strong evidence. No supplement replaces weight loss, exercise, or blood sugar control. Always talk to your doctor before taking anything.
How often should you get tested if you have NAFLD?
If you have simple fatty liver (NAFL) and no other risks, check ALT and FIB-4 every 1-2 years. If you have NASH or fibrosis, you need more frequent monitoring-every 6-12 months. FibroScan or MRI may be repeated every 1-3 years to track progression. If you’re losing weight or on medication, your doctor may test more often.
Can NAFLD turn into liver cancer?
Yes, but mostly if it progresses to cirrhosis. About 5-12% of NASH patients develop liver cancer over 10-20 years. The risk is much lower with NAFL. Regular monitoring with ultrasound every 6-12 months is recommended for anyone with stage 3 fibrosis or cirrhosis.



David Cunningham on 23 November 2025, AT 23:27 PM
Been told I have fatty liver last year. Got a FibroScan last month - 8.4 kPa. Scared the crap outta me. Started walking 45 mins daily and cut out soda. Lost 12 lbs in 3 months. My last scan was 6.9. Not fixed, but moving. Don’t wait like I did.