Clozapine ANC Monitoring Calculator
This calculator shows your next required ANC blood test based on the FDA's current monitoring guidelines. Remember: ANC monitoring remains medically required even though the REMS program is gone.
Your next ANC test is due on
Do not miss your ANC tests. Severe neutropenia occurs most frequently in the first 18 weeks of treatment.
The FDA has officially removed the mandatory REMS program for clozapine as of February 24, 2025. This isn’t just a paperwork change-it’s a major shift in how doctors and pharmacies handle one of the most effective, yet most misunderstood, medications for treatment-resistant schizophrenia. For years, patients had to jump through hoops just to get their clozapine filled. Blood tests had to be reported to a federal registry. Prescribers and pharmacies needed special certifications. If one form was late, the prescription couldn’t be filled. Now? None of that is required anymore.
What Was the Clozapine REMS Program?
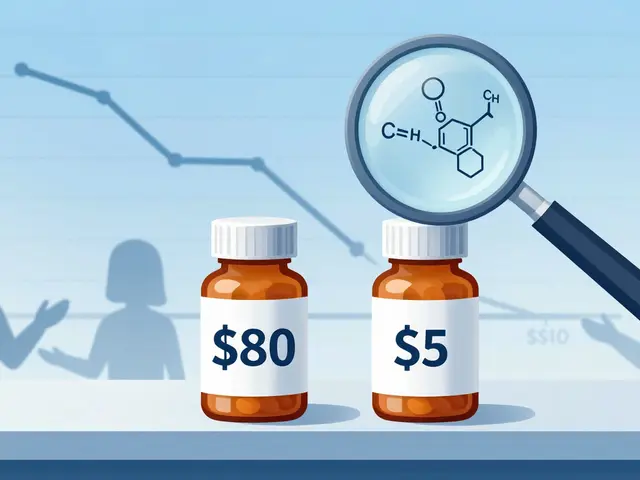
The Risk Evaluation and Mitigation Strategy (REMS) for clozapine was created because the drug carries a rare but serious risk: severe neutropenia, which can lead to agranulocytosis-a dangerous drop in white blood cells that leaves the body unable to fight infection. The risk is highest in the first 18 weeks of treatment, but it never fully disappears. In the 1990s, this led to dozens of deaths, and the FDA stepped in. By 2015, they locked clozapine into a strict monitoring system that required every prescriber, pharmacy, and patient to enroll in a federal database. Blood test results-specifically Absolute Neutrophil Count (ANC)-had to be submitted monthly before a pharmacy could dispense the next supply.It wasn’t just inconvenient. It was a barrier. Clinics spent an average of 3.2 hours a week just filing paperwork. Pharmacies added 10 to 15 minutes per clozapine prescription to verify compliance. Patients in rural areas often waited weeks because their local pharmacy wasn’t certified. A 2023 study found that 30% of eligible patients missed out on clozapine because of these delays. That’s not just a system failure-it’s a treatment failure.
Why Did the FDA Remove the REMS Program?
The FDA didn’t make this decision lightly. They spent over a year reviewing real-world data from the Sentinel System, the Department of Veterans Affairs, and Brigham and Women’s Hospital. The results were clear: doctors and pharmacists were already doing the right thing-without being forced to.Even without the REMS registry, healthcare providers continued to check ANC levels on the same schedule: weekly for the first six months, biweekly from six to 12 months, and monthly after that. The risk of severe neutropenia is still real-about 0.8% of patients develop it-but providers are now monitoring it based on medical guidelines, not government mandates. The FDA concluded that the REMS program had served its purpose. It raised awareness. It trained clinicians. It built systems. And now, those systems are working on their own.
This change sets clozapine apart from other high-risk drugs like thalidomide or isotretinoin, which still require active REMS programs. Clozapine’s safety record improved so much that the regulatory machinery became unnecessary. As the FDA put it: "The benefits of clozapine continue to outweigh its risks, and healthcare professionals are managing those risks effectively without mandatory reporting."
What Changes for Patients and Providers?
For patients: you no longer need to worry about submitting forms to a federal portal. Your doctor doesn’t have to re-certify every year. Your pharmacy won’t call you three times to confirm your ANC result was submitted. If your doctor orders a blood test, it’s because they’re following medical best practices-not because a government system is blocking your prescription.For prescribers: you’re no longer required to enroll in the Clozapine REMS website or submit monthly Patient Status Forms. Certification is no longer mandatory. But here’s the catch: you’re still expected to monitor ANC levels. The FDA hasn’t removed the risk. They’ve removed the bureaucracy. The boxed warning about severe neutropenia stays on every clozapine label. The prescribing information still says: "Monitor ANC before starting and regularly during treatment."
For pharmacies: you don’t need to be certified anymore. You can fill clozapine prescriptions without checking a federal database. But you’re still responsible for ensuring the patient is being monitored. If a patient shows up without recent ANC results, you should still ask. If they haven’t had a test in three months, you should flag it. This isn’t about compliance anymore-it’s about clinical judgment.

What About the ANC Monitoring Schedule?
The timing hasn’t changed. The medical community still follows the same proven schedule:- Before starting: Baseline ANC must be done.
- Weeks 1-18: Weekly ANC tests.
- Months 5-12: Biweekly if ANC is normal (≥1500/μL for most; ≥1000/μL for patients with Benign Ethnic Neutropenia).
- After 12 months: Monthly, using shared decision-making with the patient.
This schedule isn’t arbitrary. It’s based on decades of data showing that 90% of severe neutropenia cases occur within the first 18 weeks. After that, the risk drops sharply-but doesn’t vanish. That’s why monitoring doesn’t stop. It just becomes less frequent.
Doctors who treat schizophrenia know this. The American Psychiatric Nurses Association, the Medical Letter, and the American Society of Health-System Pharmacists all agree: ANC monitoring remains the standard of care. The difference now is that it’s guided by clinical ethics, not federal rules.
Why This Matters for People With Treatment-Resistant Schizophrenia
Clozapine isn’t just another antipsychotic. It’s the only one proven to reduce suicide risk in schizophrenia. It works when nothing else does. Meta-analyses show 30-50% of patients respond to clozapine after failing two or more other drugs. For comparison, other second-generation antipsychotics work in only 10-15% of those cases.Yet, in 2024, only about 128,000 Americans were on clozapine-even though an estimated 1.1 million have treatment-resistant schizophrenia. That’s less than 12% of those who could benefit. The REMS program was a big reason why. Clinics without dedicated REMS coordinators were 3.7 times less likely to start patients on clozapine. Now, that barrier is gone.
Analysts at Evaluate Pharma predict clozapine sales will jump from $487 million in 2024 to $612 million by 2026. That’s not because the drug got cheaper. It’s because more people can get it. Anthem’s provider network expects a 25-30% increase in new clozapine starts over the next two years. That’s thousands of people who might finally find relief after years of failed treatments.

What’s Next?
The FDA is not walking away from safety. They’re shifting from enforcement to surveillance. The Sentinel System will keep watching for signs of neutropenia. Manufacturers are updating labels to remove REMS references but keep the boxed warning. Professional groups like the American Society of Health-System Pharmacists are rolling out updated guidelines in Q3 2025 to help clinicians navigate the new landscape.Some worry this change could lead to monitoring gaps. But the data doesn’t support that fear. Studies show providers didn’t stop monitoring when REMS was in place-they just did it better. Now, they’re free to do it the way they always should have: as part of good clinical care, not as a compliance chore.
The removal of the REMS program doesn’t mean clozapine is less dangerous. It means we’ve trusted clinicians to do their job-and they’ve proven they can.
What Patients Should Do Now
If you’re on clozapine or considering it:- Don’t stop getting blood tests. Your doctor still needs to check your ANC.
- Ask your prescriber when your next test is due. Don’t wait for them to remind you.
- If your pharmacy asks for a REMS form, tell them the program was removed in February 2025.
- Report any signs of infection-fever, sore throat, fatigue-right away. These could be early signs of neutropenia.
For those who were denied clozapine because of REMS delays: your access is now open. Talk to your psychiatrist. Bring up the change. You deserve a chance at a better life.
Is clozapine still dangerous?
Yes, clozapine still carries a risk of severe neutropenia and agranulocytosis, especially in the first 6 months of use. However, the risk is low-about 0.8% based on VA data-and it’s well-managed with regular blood tests. The FDA removed the mandatory REMS program because providers have consistently monitored patients safely without federal enforcement.
Do I still need to get my ANC checked?
Yes. Even though the federal REMS program is gone, ANC monitoring is still medically required. The FDA and all major psychiatric organizations recommend weekly tests for the first 6 months, biweekly from 6 to 12 months, and monthly after that. Stopping blood tests increases your risk of undetected neutropenia.
Can my pharmacy refuse to fill my clozapine prescription now?
No, pharmacies no longer need FDA certification or proof of ANC submission to dispense clozapine. However, they should still ask if you’ve had your recent blood test. If you haven’t, they may delay filling it to protect your safety-this is now a clinical decision, not a legal requirement.
Do I need to re-enroll in the REMS program?
No. The Clozapine REMS program was officially discontinued on February 24, 2025. You are no longer required to enroll, recertify, or submit any forms to the federal registry. Any website or form asking you to do so is outdated.
Will clozapine be easier to get now?
Yes. With the REMS program gone, prescribers can start patients without bureaucratic delays. Pharmacies can fill prescriptions faster. Experts predict a 25-30% increase in clozapine use over the next two years. If you’ve been denied clozapine before because of paperwork, this is your chance to try again.



Julia Strothers on 21 November 2025, AT 08:44 AM
This is a total government power grab disguised as "relief"-they removed REMS so they can track you through your pharmacy’s EHR instead. You think they don’t know who’s on clozapine now? They’ve got your ANC data flowing into CDC databases under "public health surveillance." Wake up, sheeple. This isn’t freedom-it’s stealth monitoring.
And don’t believe the "0.8% risk" lie. That number’s cooked. The VA data? They exclude anyone who got sick and dropped out. The real death rate? At least 2x higher. They’re just not counting the bodies anymore.
They removed the registry because they don’t need it. They’ve got AI algorithms scraping your lab results now. You’re being watched. Always.
Next they’ll say "no more diabetes screenings for metformin" and then quietly start denying insulin to non-compliant patients. This is how they ration care. Slowly. Quietly. With a smile.
They told us REMS was a burden. It was our only shield.