Amiloride: What It Does and When You Might Need It
Want a clear, no-nonsense take on amiloride? This short guide explains how it works, why doctors prescribe it, what to watch for, and simple safety steps you can use right away.
Amiloride is a potassium-sparing diuretic. That means it helps your body get rid of extra fluid while keeping potassium from falling too low. Doctors often use it alongside thiazide diuretics to stop low potassium, or alone in conditions where preserving potassium matters.
Common uses and real-world tips
Here’s when amiloride shows up in real care: managing edema from heart or liver problems, treating high blood pressure when other drugs cause low potassium, and helping patients with Gitelman syndrome — a rare kidney condition that causes low potassium and magnesium. In Gitelman, amiloride can reduce urinary potassium losses and ease symptoms like muscle weakness and cramps.
Typical adult doses start low — often 5 mg once daily — and can be adjusted. It’s commonly combined with hydrochlorothiazide (as a fixed pill) so you get fluid control without big potassium drops. Always follow your prescriber’s exact dose; don’t double up if you miss one.
Side effects, interactions, and simple safety rules
Main risk: high potassium (hyperkalemia). If your kidneys aren’t working well, or you take ACE inhibitors, ARBs, spironolactone, trimethoprim, or potassium supplements, your potassium can rise dangerously. NSAIDs can also blunt kidney function and raise risk. That’s why baseline and follow-up blood tests matter.
Other common issues: dizziness (from blood pressure drop), nausea, headache, and sometimes leg cramps. Serious warning signs to call your doctor about right away include weakness, numbness, irregular heartbeat, or sudden fainting.
Practical monitoring tips: before starting get a blood test for potassium and creatinine. Repeat checks about 1 week after a dose change, then periodically based on your kidney function and other meds. If potassium goes above your target, your clinician may lower the dose or stop amiloride.
Daily habits that help: avoid salt substitutes that contain potassium, don’t take extra potassium supplements unless your doctor okays them, and tell every clinician about amiloride — especially emergency care providers.
Special cases: pregnancy and breastfeeding need a talk with your clinician. Kids and older adults may need different doses and closer monitoring. If you have diabetes or heart disease, your care team will balance the benefits and risks.
Final practical note: if you’re shopping for meds, get them from a licensed pharmacy and keep copies of your prescriptions and blood work. If anything feels off on the drug, call your provider — quick adjustments prevent bigger problems.
Questions about what to expect on amiloride? Ask your prescriber for a clear monitoring plan and a list of meds to avoid. That small checklist keeps treatment safe and effective.
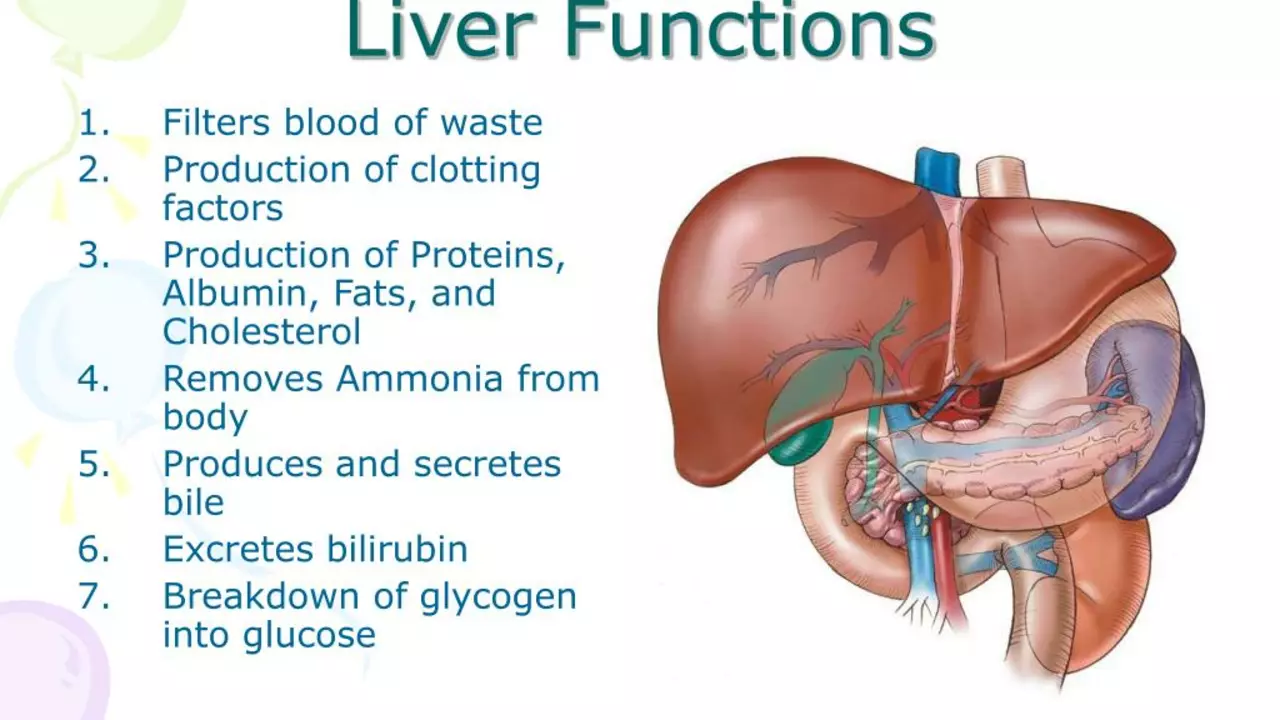
In my latest research, I delved into the effects of amiloride, a medication commonly used for heart-related conditions, on liver function in patients with hepatic impairment. It turns out that amiloride can have a significant impact. For some, it aids in managing fluid imbalances, but for others, it can potentially lead to further liver complications. This reminds us of the importance of individualized treatment plans. Overall, the impact of amiloride on liver function is a complex issue that requires further investigation.