When you pick up a prescription, you might see two options: the familiar brand name you’ve heard on TV, or a cheaper generic with a plain label. Most people assume they’re the same. But are they? And if you’re taking a medication for years - for high blood pressure, thyroid issues, or epilepsy - does it really matter which one you get?
The truth isn’t simple. For most people, generics work just fine. But for others, especially those on narrow therapeutic index drugs, the difference can be life-changing. And while regulators say generics are equivalent, real-world data tells a more complicated story.
What Does ‘Bioequivalent’ Actually Mean?
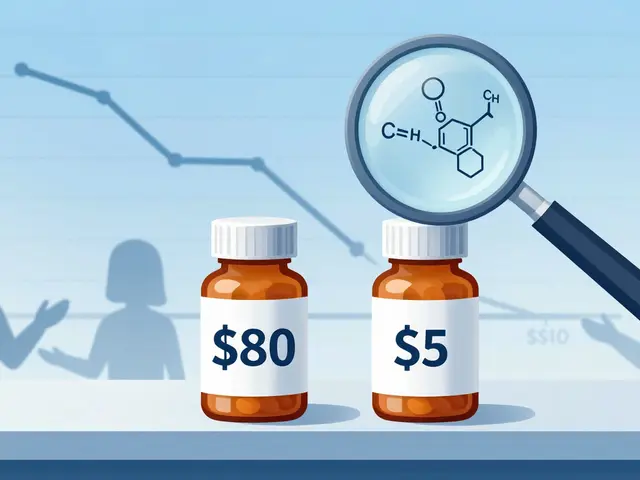
The FDA requires generics to prove they’re bioequivalent to the brand-name drug. That means the amount of active ingredient your body absorbs - measured by AUC and Cmax - must fall within 80% to 125% of the brand’s levels. Sounds strict? It is. But here’s the catch: that’s a 45% window. A generic could deliver 20% less or 25% more of the drug than the brand and still be approved.
On paper, that sounds fine. The average difference across thousands of studies is only about 3.5%. But for drugs where even a small change in blood level can cause harm - like warfarin, levothyroxine, or seizure meds - that 20% variation isn’t just a number. It’s a risk.
Take levothyroxine. A 2017 study found patients switching from Synthroid to generic versions had a 12.3% higher rate of thyroid-stimulating hormone (TSH) fluctuations. That might not sound like much, but for someone with hypothyroidism, it means fatigue, weight gain, or worse - heart rhythm problems. One small shift, over months, can add up.
Big Studies, Big Differences
In 2020, researchers in Austria looked at over 1.3 million people taking medications for chronic conditions like high blood pressure. They compared brand-name drugs to generics over five years. The results shocked many.
People on brand-name antihypertensives had 53.8 deaths per 1,000 patient-years. Those on generics? Just 30.2. That’s nearly half the death rate. Major cardiac events like heart attacks and strokes were also nearly 40% lower in the generic group. After adjusting for age, income, and other factors, the advantage for generics held strong.
Wait - generics were safer?
Yes. And the study didn’t stop there. They checked for bias. Did people on generics have healthier lifestyles? Were they younger? No. They used advanced statistical methods to rule out confounding factors. The conclusion: generics weren’t just as safe - they were better.
But here’s where it gets messy.
The Other Side of the Coin
Not every study agrees. Some patients report dramatic drops in effectiveness after switching. There’s a documented case of someone on generic ciprofloxacin whose infection didn’t clear - until they switched back to the brand. Another person on generic levofloxacin kept running a fever until they went back to Tavanic. Symptoms vanished within days.
One 2013 analysis found that about 30% of patients saw no change after switching. Another 30% improved. But 30% had worse symptoms or stopped taking the drug entirely. That’s a lot of people affected.
Why does this happen? It’s not always the active ingredient. It’s the fillers. The coating. The way the pill breaks down in your stomach. These inactive ingredients - called excipients - aren’t required to match the brand. But they can affect how quickly or completely the drug is absorbed.
For someone with Crohn’s disease, a sensitive gut, or poor stomach acid, that difference matters. A pill that dissolves too slowly might not work. One that dissolves too fast might cause nausea or spikes in blood levels.
Who Makes the Generic Matters More Than the Label
Here’s something most people don’t realize: the same company that makes the brand-name drug often makes the generic too. These are called authorized generics. They’re identical in every way - same factory, same formula, just a different label.
Now look at adverse event reports. For amlodipine (a blood pressure drug), 56% of reports came from generic versions, 29% from the brand. But when you compare authorized generics to regular generics? The numbers look almost the same. That suggests the problem isn’t ‘generic’ - it’s ‘made by Company X’.
A 2018 Ohio State study found something even more telling. Generic drugs made in India had 54% more severe adverse events - including hospitalizations and deaths - than those made in the U.S. The difference was strongest for older, well-established drugs like ciprofloxacin. Indian-made versions led to 62% more hospitalizations due to side effects.
This isn’t about quality control alone. It’s about oversight. The FDA inspects fewer foreign plants than domestic ones. And with thousands of generic manufacturers worldwide, tracking every batch is nearly impossible.
What About the FDA’s Data?
The FDA says generics are safe. And they have data to back it up. A 2021 Harvard study tracked over 136,000 seniors on three blood pressure drugs - losartan, valsartan, and candesartan. When generics entered the market, ER visits and hospitalizations didn’t go up. Not even slightly.
But here’s the flaw in that study: it only looked at serious events. It didn’t catch mild side effects - dizziness, headaches, fatigue - that might make someone stop taking the drug. And it didn’t track long-term outcomes like kidney damage or stroke risk over five or ten years.
Also, the FDA’s own adverse event database shows 1,247 reports between 2018 and 2022 saying ‘generic drug ineffective.’ Only 289 for brand-name drugs. That’s over four times more complaints. And remember: most people don’t report side effects. So this is just the tip of the iceberg.

Who Should Be Careful?
Not everyone needs to worry. For antibiotics, painkillers, or antihistamines, generics are almost always fine. But for certain drugs, the stakes are higher:
- Levothyroxine - tiny changes in dose affect metabolism, heart rate, mood
- Warfarin - a 10% change in blood level can cause dangerous bleeding or clots
- Anti-seizure drugs - lamotrigine, phenytoin, carbamazepine
- Immunosuppressants - cyclosporine, tacrolimus - used after transplants
- Psychiatric meds - lithium, some SSRIs
These are called narrow therapeutic index drugs. The line between effective and toxic is thin. And generics aren’t always consistent across batches or manufacturers.
Reddit has hundreds of posts like this: ‘Switched from Lamictal to generic. Seizures went from 1-2/month to 8-10. Switched back - stopped immediately.’ That’s not anecdotal. That’s a pattern.
What Should You Do?
You don’t need to avoid generics. But you do need to be smart.
- Ask your pharmacist - which manufacturer made your generic? If you’ve had issues before, ask to stick with the same one.
- Don’t switch randomly - if your blood pressure or thyroid levels are stable, don’t let your insurer force you to switch unless you’re told why.
- Track your symptoms - keep a simple log: energy, mood, heart rate, side effects. If things change after a switch, talk to your doctor.
- Know your drug’s therapeutic index - if it’s on the list above, be extra cautious.
- Check the FDA’s list - some generics are approved as ‘therapeutically equivalent’ (AB-rated). Others aren’t. Ask your pharmacist to check.
And if you’re on a high-risk drug and your insurance pushes you to a cheaper generic? Push back. Say: ‘I’ve been stable on this version. I need to stay on it.’ You have the right to request a brand if it’s medically necessary.
The Bigger Picture
Generics saved the U.S. healthcare system over $300 billion in 2022. That’s huge. They make medicine affordable. But affordability shouldn’t mean guessing whether your drug will work.
The system works for most people. But for the 10-15% who are sensitive to small changes - the elderly, the chronically ill, those on complex meds - it’s not enough. We need better monitoring. Better testing. Better transparency about who makes what.
Until then, knowledge is your best tool. Don’t assume generics are always the same. Don’t assume brands are always better. Just know: your body might react differently - and that’s okay. Track it. Talk about it. And don’t let cost override safety.





Robyn Hays on 29 December 2025, AT 01:25 AM
Wow. This post is a masterclass in nuance. I’ve been on levothyroxine for 12 years, and I switched generics three times before I realized my fatigue wasn’t just ‘aging’-it was my thyroid acting up. I started tracking my TSH levels and symptoms in a spreadsheet. Turns out, the generic from Teva made me feel like a zombie; the one from Mylan? I could run marathons. It’s not about brand loyalty-it’s about batch consistency. And yeah, the fillers matter. My gut is basically a petri dish for pharmaceutical drama.