Endometrial Health – Why the Uterine Lining Matters
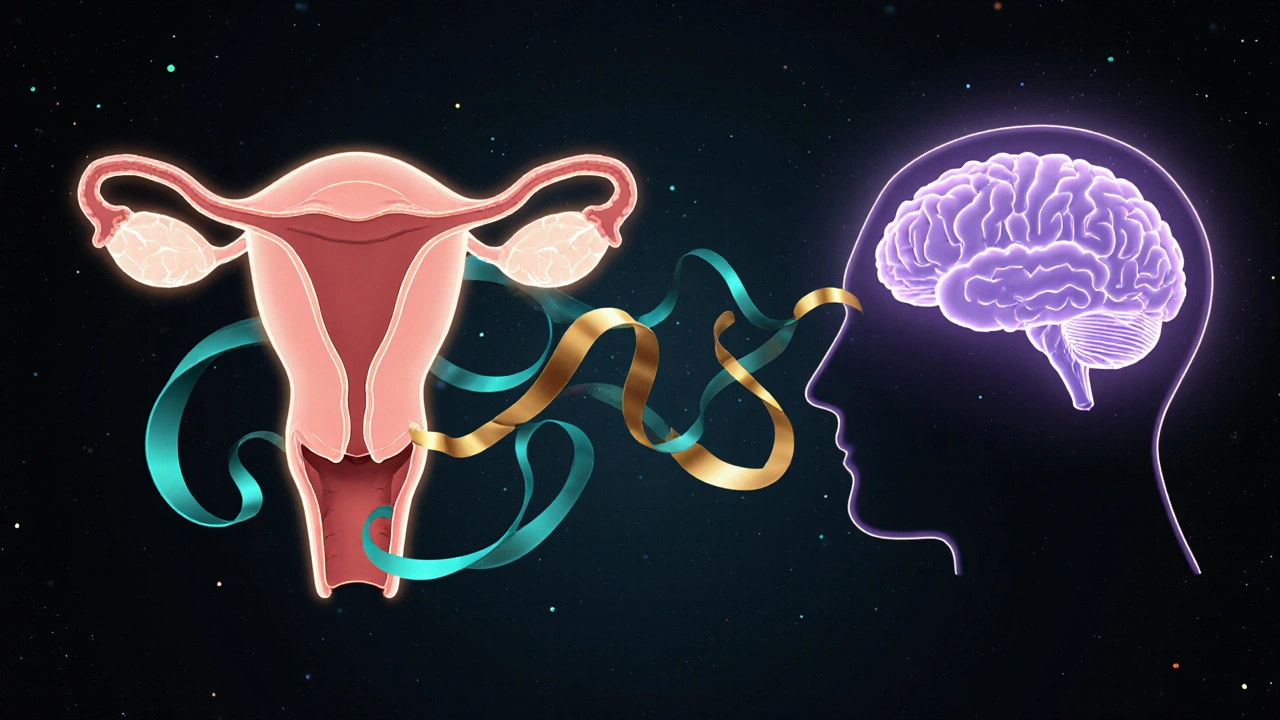
When talking about Endometrial Health, the condition and overall wellbeing of the uterine lining, which influences fertility, menstrual cycles, and disease risk. Also known as uterine lining health, it is a core indicator of a woman's reproductive system. Good endometrial health means the lining can thicken and shed as needed, supporting implantation and regular periods. Poor health can lead to heavy bleeding, infertility, or even precancerous changes. Understanding how hormones, medications, and lifestyle choices interact with the endometrium helps you stay ahead of problems before they become serious.
Key Factors Influencing Endometrial Health
One of the biggest drivers is Hormone Therapy, the use of estrogen and progesterone to manage menopausal symptoms or address hormonal imbalances. Estrogen encourages the lining to grow, while progesterone signals it to stabilize and later shed. When these hormones are out of balance, the endometrium can become too thick (hyperplasia) or too thin, each with its own risks. Tamoxifen, a selective estrogen receptor modulator commonly prescribed for breast cancer that also stimulates the uterine lining is another frequent culprit; many patients on tamoxifen notice irregular bleeding and need monitoring. Age‑related changes, especially during Menopause, bring natural declines in estrogen, often resulting in a thinner lining and more spotting. Lifestyle matters, too – obesity raises estrogen levels because fat tissue converts androgens, while smoking can impair blood flow to the uterus. Stress, diet, and exercise also sway hormone production, making them indirect but powerful levers for endometrial health.
Clinicians use a few practical tools to gauge how the endometrium is doing. Ultrasound thickness measurement is the first line; a lining under 5 mm after ovulation may suggest insufficient estrogen, while a lining over 12 mm in a postmenopausal woman raises alarm for hyperplasia. Endometrial biopsy takes a tiny tissue sample to check for abnormal cells, especially after long‑term tamoxifen use. Blood tests for hormone levels (estradiol, progesterone, FSH, LH) give a broader picture of the endocrine environment. When issues are spotted, treatment options range from adjusting hormone doses, switching tamoxifen to an alternative, or prescribing a progestin‑only regimen to thin an overgrown lining. Even simple changes—weight loss, quitting smoking, adding a balanced diet rich in omega‑3s—can rebalance hormones naturally. Below, you’ll find articles that break down these topics, compare medications, and share step‑by‑step guides for buying safe, affordable generics that affect endometrial health. Dive in to see how each piece fits into the bigger picture of keeping your uterine lining in top shape.
Learn how endometrial hyperplasia, the overgrowth of the uterine lining, can trigger mood swings, anxiety, and depression, and discover practical steps to manage both the condition and its emotional effects.