Endometrial Hyperplasia Mood: What You Need to Know
When talking about endometrial hyperplasia mood, the emotional changes that accompany the thickening of the uterine lining. Also known as uterine lining mood swings, it often overlaps with endometrial hyperplasia, a condition where estrogen‑driven growth makes the endometrium unusually thick. This hormonal imbalance can trigger mood disorders, such as depression, anxiety or irritability, especially when estrogen levels stay high for long periods. Hormonal therapy, treatments that balance estrogen and progesterone plays a key role in easing both the tissue changes and the associated emotional symptoms. Understanding how estrogen, the primary driver of endometrial growth influences mood helps you spot patterns early and choose the right care.
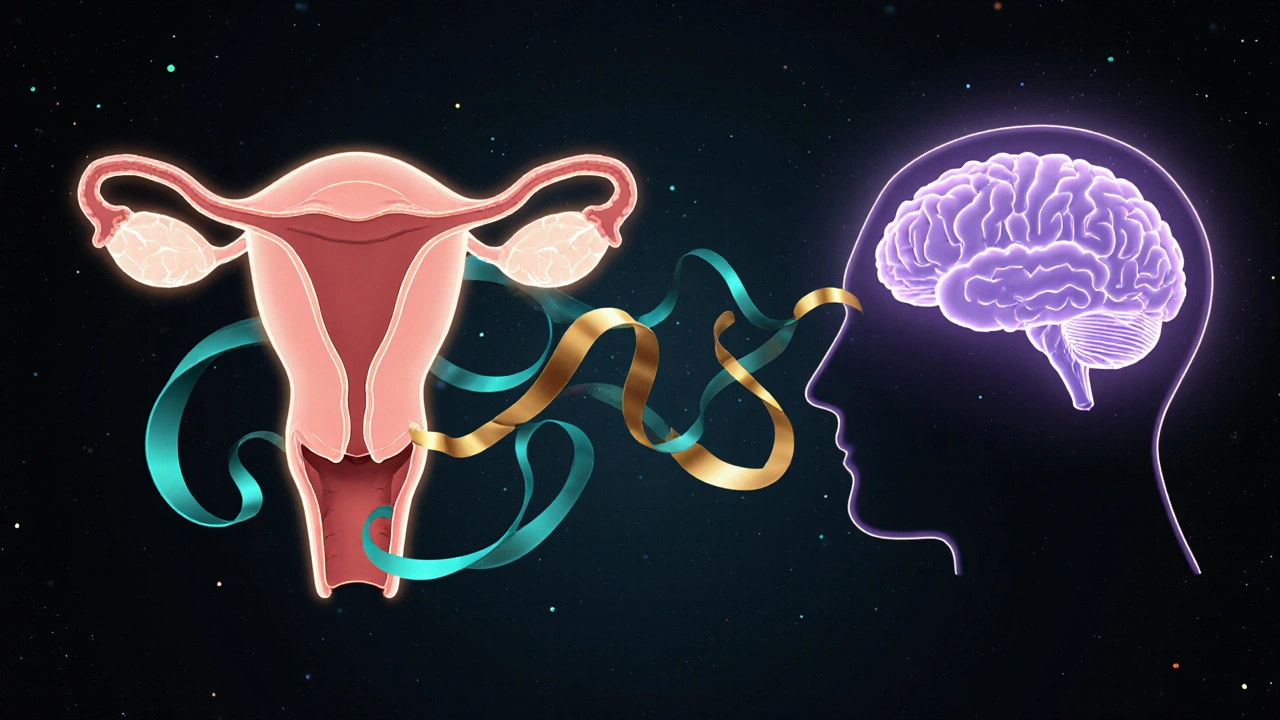
Why Hormones Affect Both the Uterus and Your Feelings
Estrogen isn’t just a reproductive hormone; it talks to brain regions that regulate serotonin and dopamine. When estrogen spikes, you might feel energetic, but prolonged excess can wear down those neurotransmitter pathways, leading to low mood or anxiety. Progesterone, on the other hand, has a calming effect. In many cases of endometrial hyperplasia, progesterone levels are insufficient, so the brain misses that soothing signal. This hormonal tug‑of‑war creates a feedback loop: the uterus thickens, the brain feels off‑balance, and mood swings worsen. Recognizing this link is the first step toward breaking the cycle.
Symptoms often hide behind everyday complaints. A woman might attribute fatigue, irritability, or night‑time crying to stress at work, not realizing her endometrial lining is the hidden culprit. Common physical signs—irregular bleeding, spotting between periods, or unusually heavy periods—can coincide with emotional turbulence. When both sets of symptoms appear together, clinicians should consider the hormonal connection rather than treating them separately.
Management strategies aim at two fronts: shrinking the thickened lining and stabilizing mood. Progestin‑based oral medications, intrauterine devices releasing levonorgestrel, or even low‑dose oral contraceptives can reverse hyperplasia in many cases. At the same time, lifestyle tweaks—regular exercise, balanced diet rich in omega‑3 fatty acids, and stress‑reduction techniques—support brain chemistry. If mood symptoms persist, a short course of antidepressants or counseling may be added, but always alongside hormonal treatment to address the root cause.
Knowing the interplay between endometrial hyperplasia and mood equips you to ask the right questions at your next appointment. Look for explanations that tie bleeding patterns to emotional shifts, and be ready to discuss hormonal therapy options that target both issues. Below, you’ll find articles that break down the science, compare treatment choices, and share practical tips for coping with the emotional side of this condition.
Learn how endometrial hyperplasia, the overgrowth of the uterine lining, can trigger mood swings, anxiety, and depression, and discover practical steps to manage both the condition and its emotional effects.