Fatty Liver: Causes, Risks, and What You Can Do About It
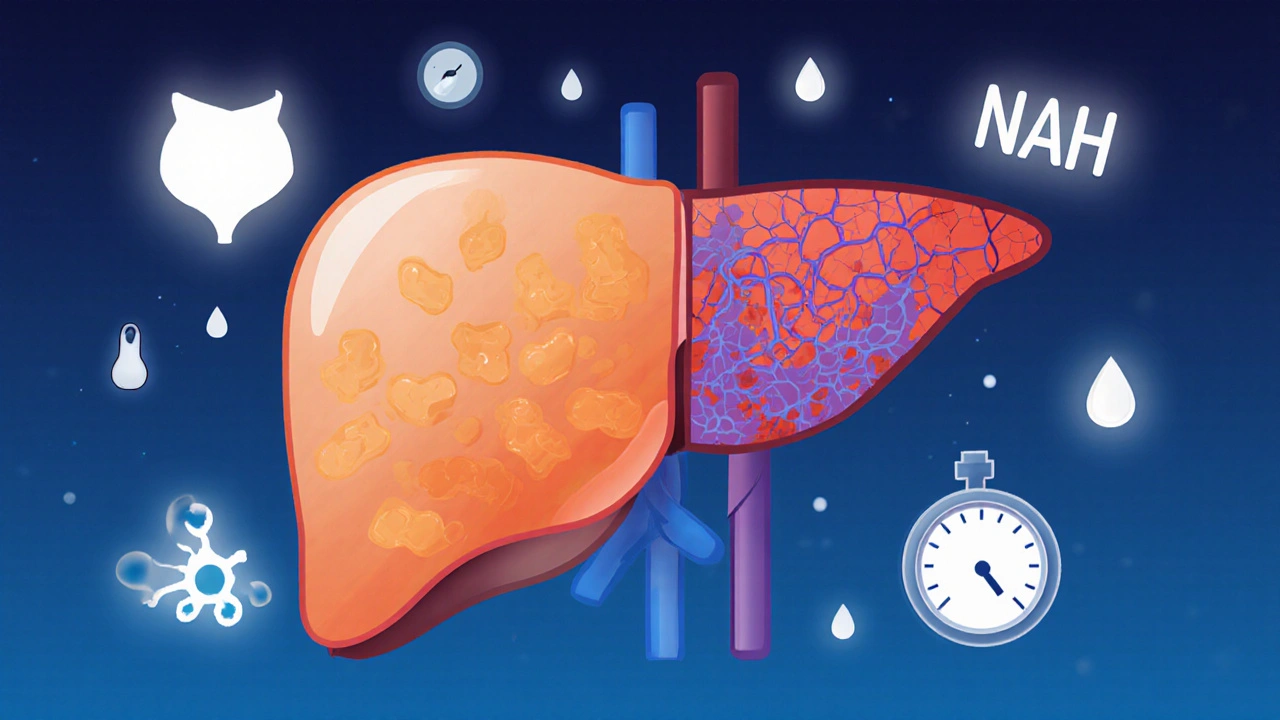
When your liver stores too much fat, it’s called fatty liver, a condition where excess fat builds up in liver cells, often without symptoms until damage occurs. Also known as hepatic steatosis, it’s not just a result of drinking too much—it’s deeply tied to how your body handles sugar, fat, and insulin. About 25% of adults worldwide have some form of fatty liver, and most don’t know it. The scary part? It can quietly turn into inflammation, scarring, or even liver failure if ignored.
Fatty liver comes in two main types: one linked to alcohol, and the other—more common—to metabolic issues like insulin resistance, a condition where cells stop responding well to insulin, leading to high blood sugar and fat storage in the liver. This second type, called non-alcoholic fatty liver disease (NAFLD), is growing fast because of diets high in sugar and processed carbs, sedentary habits, and obesity. It’s not rare in people who aren’t overweight either—some have it because of genetics or gut health problems. What ties these cases together? Your liver gets overwhelmed trying to process too much fat and sugar, and it starts storing the excess instead of burning it.
What makes fatty liver dangerous isn’t the fat itself—it’s what happens next. Fat in the liver can trigger inflammation, which turns into non-alcoholic steatohepatitis, a more serious form of fatty liver that causes liver cell damage and can lead to cirrhosis. And here’s the catch: you won’t feel it until it’s advanced. No pain, no jaundice, no obvious signs. Blood tests might show slightly high liver enzymes, but often they’re normal. That’s why so many people only find out after a routine scan or when complications show up.
The good news? Fatty liver is often reversible—especially in the early stages. Cutting back on sugar, losing even 5-10% of body weight, and moving more can shrink liver fat significantly. Some studies show that just 30 minutes of brisk walking five days a week reduces liver fat more than some medications. You don’t need a miracle diet or expensive supplements. Real change comes from consistent habits: swapping soda for water, eating more vegetables, and avoiding late-night snacks. Even small shifts matter.
And while medications are being studied, right now the best treatment is lifestyle. No pill replaces movement. No supplement fixes a diet full of refined carbs. The posts below show you exactly how fatty liver connects to other health issues—like heart disease, diabetes, and even how certain meds can make it worse. You’ll find clear guides on what to eat, what to avoid, how to monitor your liver health without expensive tests, and what to ask your doctor if you’ve been told you have it. This isn’t about fear—it’s about knowing what’s really going on and taking control before it’s too late.
NAFLD and NASH are part of the same liver spectrum-simple fat buildup vs. inflamed, damaged liver tissue. Understanding fibrosis risk is key to preventing cirrhosis and liver cancer. Early action can reverse damage.