Hepatic impairment: how liver problems change your medicines
A small drop in liver function can change how a drug behaves in your body. That matters because the liver handles breakdown for many common meds — from blood thinners to painkillers and some sleep drugs. If the liver slows down, a usual dose can build up and cause harm. This page gives clear, practical steps so you and your healthcare team can stay safer with medicines.
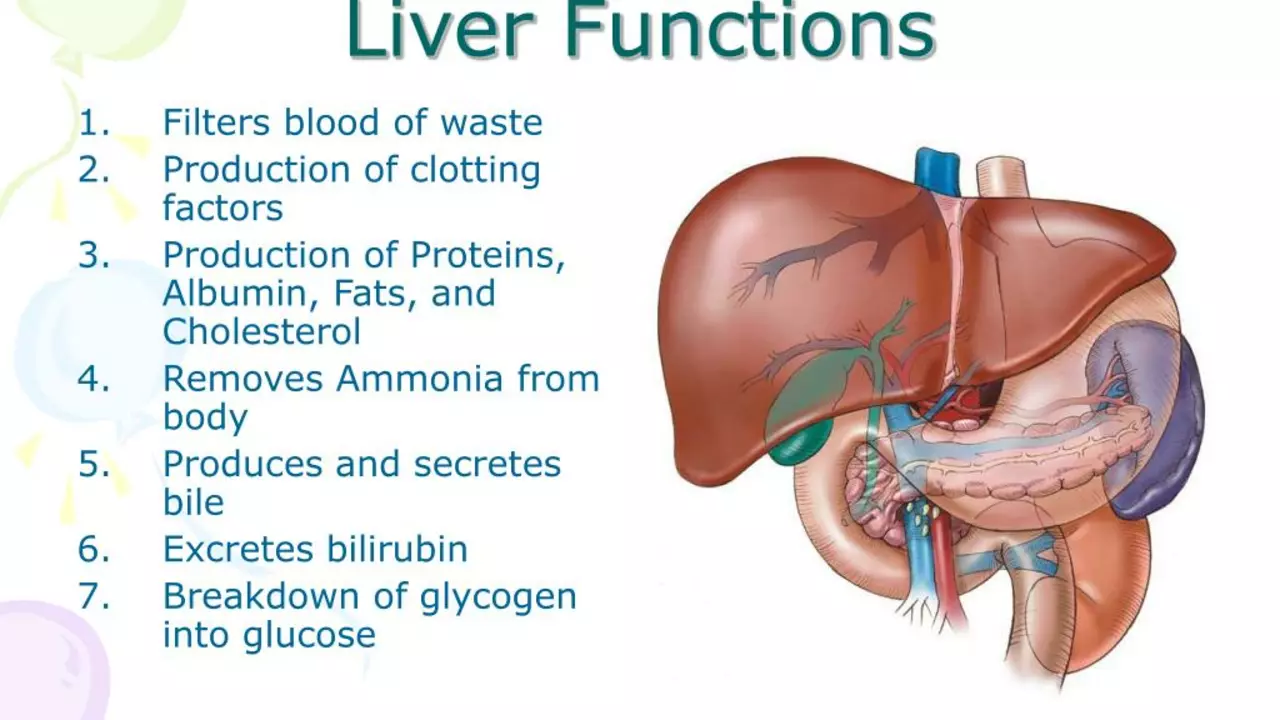
Why the liver matters for drugs
The liver does three important things for medications: it breaks them down (metabolism), helps drugs stick to proteins in the blood (protein binding), and clears the by-products. When liver function drops, drug levels can go up, effects can last longer, and side effects can grow. For example, drugs that rely on CYP enzymes (a common liver pathway) — like many statins, some anti-seizure meds, and certain antidepressants — often need a lower dose or slower schedule when liver function is poor.
Clinicians usually use simple tools like the Child-Pugh score to describe how bad liver disease is. Child-Pugh sorts patients into A (mild), B (moderate), and C (severe). Many medication guides give dosing changes based on these categories — lower starting doses, longer time between doses, or avoiding the drug entirely in severe cases.
Practical tips for patients and caregivers
Keep a clear, updated list of everything you take — prescriptions, over-the-counter pills, vitamins, and herbal supplements. Bring that list to every visit and ask: “Does my liver change how I should take this?” Pharmacists can often spot risky combos or drugs that need dose changes.
Watch the simple warning signs: yellow eyes or skin (jaundice), new belly swelling, heavy bruising or bleeding, increasing sleepiness or confusion (could signal hepatic encephalopathy). If these appear after starting a new drug, stop and contact your doctor right away.
Avoid alcohol and be careful with acetaminophen (paracetamol). Even standard doses of acetaminophen can be risky for some people with liver disease — check with your clinician first. Also tell your provider about herbal products; some can harm the liver or change drug levels.
Monitoring matters. Expect your provider to check liver tests (ALT, AST, bilirubin, albumin) and sometimes INR. For drugs like warfarin, INR changes when liver function changes, so dosing may need quick adjustment. If you’re started on a medicine known to stress the liver, ask how often labs will be repeated.
When in doubt, start low and go slow. Many clinicians prefer a lower initial dose and gradual increases while watching symptoms and lab values. That approach keeps benefit and cuts risk.
If you have liver disease, be proactive: keep follow-up appointments, share your full medicine list, ask specific dosing questions, and report new symptoms fast. A little caution up front prevents big problems later.
In my latest research, I delved into the effects of amiloride, a medication commonly used for heart-related conditions, on liver function in patients with hepatic impairment. It turns out that amiloride can have a significant impact. For some, it aids in managing fluid imbalances, but for others, it can potentially lead to further liver complications. This reminds us of the importance of individualized treatment plans. Overall, the impact of amiloride on liver function is a complex issue that requires further investigation.