Myasthenia Gravis — What You Need to Know Right Now
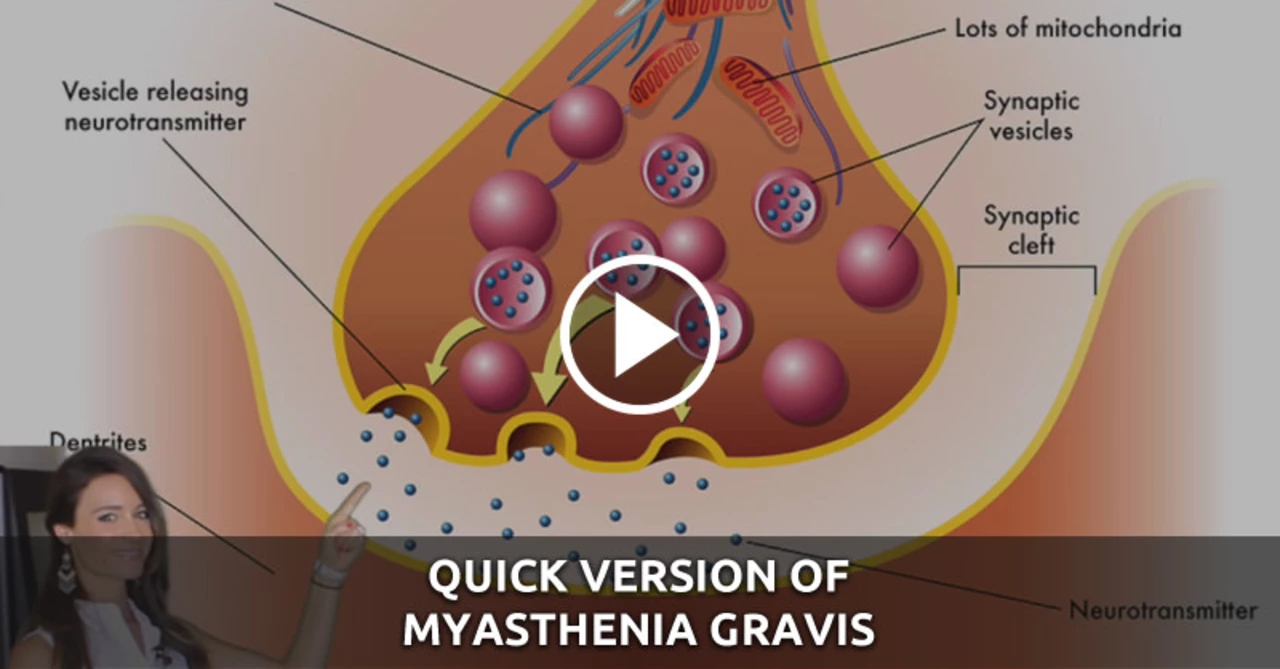
Myasthenia gravis (MG) is a condition that makes your muscles tire easily. That weakness usually shows up in the eyes, face, throat, and sometimes the limbs. Many people notice droopy eyelids, double vision, slurred speech, or trouble swallowing. The key thing to remember: symptoms often get worse with activity and improve after rest.
Diagnosis and common tests
If you suspect MG, start with a neurologist. Diagnosis is usually straightforward when you know what to look for. Doctors check for specific antibodies in the blood — most people have acetylcholine receptor (AChR) antibodies or, less often, MuSK antibodies. Electromyography (EMG) tests the neuromuscular junction and can confirm the problem when antibodies are negative. In some cases imaging (a chest CT) is done to look for a thymoma — a tumor of the thymus that can be linked to MG.
Treatment options and day-to-day tips
Treatment aims to reduce symptoms fast and control the immune attack long term. Pyridostigmine (Mestinon) helps most people by boosting muscle function. Short courses of steroids (prednisone) and steroid-sparing immunosuppressants like azathioprine or mycophenolate are common. For sudden worsening or before surgery, doctors use IVIG or plasmapheresis to pull antibodies out of the blood quickly. Thymectomy — removing the thymus — helps many people, especially younger patients and those with thymoma.
Watch for medicines that can make MG worse: some antibiotics (like aminoglycosides), certain heart drugs, magnesium supplements, and some anesthetics. Always mention MG to any new doctor and to the pharmacist. Carry a card or note that says you have myasthenia gravis and list safe emergency contacts.
Myasthenic crisis is a real emergency. If breathing becomes hard or you can’t swallow saliva, go to the ER. Intensive care with breathing support and quick treatments like IVIG or plasmapheresis can be lifesaving.
Living with MG means pacing and planning. Break tasks into short efforts and rest between them. Speech and swallow therapists can teach strategies to eat safely. Physical therapy helps keep muscles as strong and flexible as possible without overdoing it. Vaccinations are usually recommended, but check timing with your neurologist, especially if you're on immunosuppressants.
Pregnancy and MG need extra planning. Many treatments can be adjusted safely, but talk to your neurologist and obstetrician before trying to conceive. Travel is usually fine if you pack medications, a written treatment plan, and contacts for local care.
Follow-up matters. Regular check-ins let your team adjust meds and catch side effects early. Small changes in strength or breathing should prompt a quick call to your care team, not worry on your own.
If you want more practical tips or plain-language guides about MG medications and safe pharmacies, check posts on this site tagged "myasthenia gravis" for deeper reads and real-world advice.
Myasthenia Gravis has often left me struggling to get a good night's sleep, but I've discovered some tips to help achieve a more restful slumber. I found that maintaining a consistent sleep schedule and creating a comfortable sleep environment significantly improved my sleep quality. It's also important to avoid caffeine and alcohol close to bedtime, as they can disrupt the sleep cycle. Practicing relaxation techniques before bed, such as deep breathing or meditation, can help calm the mind and prepare the body for sleep. Lastly, discussing sleep issues with a healthcare professional can provide additional guidance and support.