It starts with a red, itchy rash where you applied your cream. You think it’s getting better-until it gets worse. You double down on the treatment, maybe even add another ointment. Days pass. The itching doesn’t stop. The skin burns. It spreads. You’re not improving. You’re getting worse. And you have no idea why.
This isn’t rare. In fact, it’s more common than most doctors admit. Around 1 in 6 people who get patch tested for stubborn skin rashes turn out to be allergic to the very medication they were told to use. Topical medications-creams, ointments, gels, even wipes-are supposed to heal. But for thousands, they’re the cause of the problem.
What’s Really Going On With Your Skin?
Not all skin reactions are the same. If your skin turns red and stings after using a hand sanitizer or soap, that’s irritant contact dermatitis. It’s not an allergy. It’s just damage. Your skin’s barrier got worn down. Simple. But if you’ve used the same steroid cream for weeks and suddenly your rash flares up worse than before? That’s allergic contact dermatitis. It’s your immune system flipping out. You’ve been exposed before. Your body learned to recognize the chemical. Now, even a tiny bit triggers a delayed reaction.
This isn’t a one-time thing. It builds up. You might use a prescription cream for eczema for months. Then one day-boom. Red, blistering, oozing skin where you applied it. You didn’t change anything. You followed instructions. So why now? Because your immune system finally said, “Enough.”
These Are the Most Common Culprits
It’s not just one drug. There are over 360 medications that can cause this. But a few stand out.
- Neomycin-found in over-the-counter antibiotic creams like Neosporin. It’s in nearly 10% of all positive patch tests. People think it’s helping. It’s actually making their rash worse.
- Bacitracin-another common antibiotic in topical products. About 7.5% of allergic reactions come from this.
- Corticosteroids-yes, the very drugs doctors prescribe to calm inflammation. About 0.5% to 2.2% of people using them develop an allergy. That’s a cruel twist: the treatment becomes the trigger.
- Benzocaine-a local anesthetic in numbing sprays and gels. Used for sunburns, hemorrhoids, even teething babies. Turns out, it’s a sneaky allergen.
- Ketoprofen-a topical NSAID used for muscle pain. One in 50 people who use it end up allergic.
And here’s the kicker: many of these aren’t just in prescriptions. They’re in drugstore creams, baby wipes, diaper rash ointments, and even sunscreen. You’re not just allergic to your doctor’s prescription. You’re allergic to the stuff you bought without thinking twice.
How Do You Know It’s an Allergy-and Not Just a Bad Reaction?
Most doctors won’t test you unless you push for it. They’ll assume it’s eczema flaring, fungal infection, or poor hygiene. But if your rash keeps coming back in the same spot-even after stopping the cream-you should suspect an allergy.
The gold standard is patch testing. It’s not a needle. It’s small patches stuck to your back with suspected allergens. You wear them for 48 hours. Then they’re removed. You come back at 72 hours and again at 96 hours. The doctor looks for redness, swelling, tiny blisters. That’s your immune system screaming.
It works about 70% of the time when done right. But here’s the problem: many clinics don’t test for all the common medication allergens. They use a basic panel. Neomycin? Yes. But what about the newer steroids? Or the preservatives in the cream? You need a full panel-30+ allergens at minimum. Ask your dermatologist if they use the International Contact Dermatitis Research Group standard. If they don’t, find someone who does.

The Steroid Paradox: When Your Treatment Turns Against You
This is the most confusing part. You’re told to use hydrocortisone for your rash. It helps at first. Then it stops helping. Then it makes things worse. You think you’re tolerant. You’re not. You’re allergic.
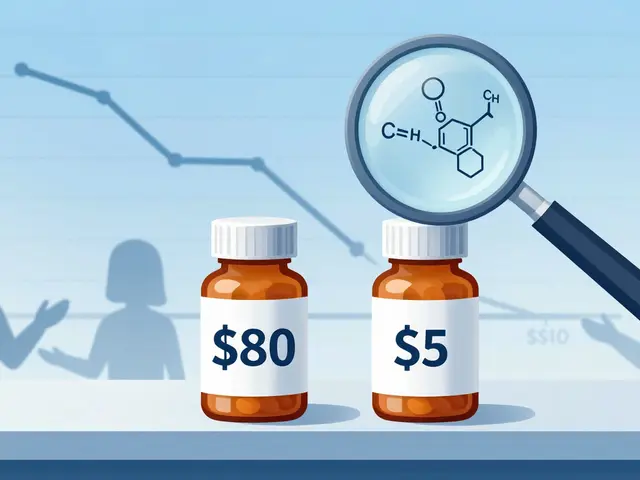
Corticosteroids are grouped into six categories based on their chemical structure. If you’re allergic to Group A (like hydrocortisone), you can usually use Group B (triamcinolone) or Group D (methylprednisolone aceponate) without issue. That’s a 65% reduction in treatment limits-if you know your group.
But most doctors don’t track this. They just switch to a “stronger” steroid. And that’s why so many patients end up with chronic rashes. They’re being treated with the wrong version of the same thing.
Studies show that when patients avoid their specific allergen, 89% of chronic cases clear up in four weeks. Without avoidance? Only 32% improve. That’s not a coincidence. That’s proof.
What to Do When You’re Allergic
First: stop the offending product. Not just the prescription. Everything. Creams, lotions, wipes, even the soap you use on the affected area. Cross-contamination is real.
Second: get tested. Don’t wait. The longer you keep exposing yourself, the more your skin remembers the allergen. It becomes harder to treat.
Third: find alternatives. For mild cases, over-the-counter hydrocortisone (0.5-1%) might still be safe-if you’re not allergic to it. But if you are, here’s what works:
- Tacrolimus (Protopic) and pimecrolimus (Elidel)-these are calcineurin inhibitors. They’re not steroids. They calm inflammation without thinning the skin. 60-70% of patients see improvement within two weeks. Side effect? A brief burning sensation when you first apply it. It fades.
- Barrier creams-newer products with ceramides and fatty acids help rebuild your skin’s natural shield. Some are designed to block allergens from penetrating. Clinical trials show up to 73% reduction in allergen exposure.
- Prescription-free moisturizers-look for fragrance-free, dye-free, preservative-free. Even “natural” products can contain plant extracts that trigger reactions. Stick to basic ones like Cetaphil, Vanicream, or CeraVe.
For severe cases-rashes covering more than 20% of your body-you’ll need oral steroids like prednisone. It works fast. Most people feel better in 12-24 hours. But it’s a band-aid. The real fix is avoiding the allergen.
What Most People Miss
You think you’re being careful. You read labels. But here’s what no one tells you: ingredients change. A cream that was safe last year might have a new preservative now. A generic version might use a different filler. You need to check every time.
Bring every product you use to your dermatologist. Not just the prescription. The lotion you use on your arms. The baby wipe you use for cleaning. The sunscreen you apply before going out. Thirty percent of allergens are found in products you don’t even think of as “medications.”
And if you’re a healthcare worker? You’re at higher risk. One in five nurses and doctors develop contact dermatitis from topical meds they handle daily. If you’re constantly washing your hands or wearing gloves, your skin barrier is already weak. Add in neomycin or bacitracin from patient care? That’s a recipe for disaster.
What’s New in 2026
The field is changing. In 2023, the FDA required full ingredient lists on all topical prescriptions. That’s helped cut misdiagnosis by 15%. Now, you can actually see what’s in your cream.
There’s also a new diagnostic tool called the Topical Medication Allergy Score. It uses 12 specific clues-like how the rash looks, where it appears, whether it worsens with reapplication-to predict allergy risk with 89% accuracy. That’s up from 65% just a few years ago.
And researchers are working on something even bigger: a blood test that could predict your risk before you even use a medication. The NIH is funding it. Early results look promising. In five years, you might get screened for topical allergies the same way you get tested for penicillin.
Real Stories, Real Pain
On Reddit, one person wrote: “I used hydrocortisone for my eczema for three years. Then my skin started peeling. I thought I was getting worse. I kept using it. By the time I stopped, my face was raw. I cried for weeks.”
Another said: “I went to five doctors. They all said ‘eczema.’ I was on six different steroid creams. Nothing worked. Patch testing finally showed I was allergic to neomycin and bacitracin. I’d been using Neosporin on my cuts for 15 years. I didn’t even know it was in there.”
These aren’t outliers. They’re the rule. The average person sees 3.2 doctors before getting the right diagnosis. It takes six months. That’s six months of burning skin, sleepless nights, and feeling like you’re broken.
You’re not broken. You just had the wrong treatment.
Final Advice: Don’t Guess. Test.
If your skin reaction keeps coming back-especially where you apply medication-get patch tested. Don’t wait. Don’t assume it’s “just irritation.” Don’t keep trying stronger steroids. You’re not fixing it. You’re feeding it.
Ask your dermatologist:
- Do you test for topical medication allergens?
- Do you use the full International Contact Dermatitis Research Group panel?
- Can you check my products for hidden allergens?
And if they say no? Find someone who will.
Your skin isn’t just a surface. It’s a barrier. And when it’s betrayed by the very things meant to heal it, you need answers-not more cream.



Juan Reibelo on 23 January 2026, AT 23:59 PM
Okay, I’ve been using Neosporin on every little cut for years. Like, every. Single. One. I thought it was helping. Turns out, my chronic eczema flare-ups? Probably that. I’m getting patch tested next week. If this is it… I’m never touching antibiotic cream again. Ever.