If you’ve been prescribed dabigatran, you’re probably wondering what it does, why your doctor chose it, and how to take it safely. You’re not alone. Thousands of people take this medication every day to prevent dangerous blood clots, but many don’t fully understand how it works or what to watch out for. This guide cuts through the confusion and gives you clear, practical information - no medical jargon, no fluff.
What is dabigatran?
Dabigatran is the active ingredient in the brand-name drug Pradaxa. It’s an anticoagulant, commonly called a blood thinner. But it doesn’t actually thin your blood. Instead, it blocks a protein in your body called thrombin, which is needed for clots to form. By slowing down clotting, dabigatran reduces your risk of stroke, especially if you have atrial fibrillation - an irregular heartbeat that can let clots form in your heart.
Before dabigatran, most people took warfarin for this. Warfarin required frequent blood tests and strict diet changes. Dabigatran changed that. It works the same way but doesn’t need regular monitoring. You take it by mouth, usually twice a day, and it starts working within hours.
Why would your doctor prescribe it?
Your doctor may have chosen dabigatran if you have one or more of these conditions:
- Atrial fibrillation (AFib) - the most common reason
- A past deep vein thrombosis (DVT) or pulmonary embolism (PE)
- Recent hip or knee replacement surgery, to prevent clots during recovery
For people with AFib, dabigatran lowers stroke risk by about 35% compared to no treatment. Studies show it’s just as effective as warfarin at preventing strokes but causes fewer dangerous brain bleeds. That’s why it’s now a first-choice option for many patients.
How do you take dabigatran correctly?
Getting the dose right matters. Dabigatran comes in 75 mg and 150 mg capsules. Most adults take 150 mg twice daily. If you’re over 80, have kidney problems, or are at higher risk of bleeding, your doctor might lower it to 75 mg twice daily.
Here’s how to take it right:
- Take it at the same times each day - morning and evening.
- Swallow the capsule whole. Don’t open, crush, or chew it.
- You can take it with or without food, but taking it with food helps reduce stomach upset.
- If you miss a dose and it’s less than 6 hours until your next one, skip the missed dose. Don’t double up.
- Never stop taking it without talking to your doctor. Stopping suddenly can increase your stroke risk.
Some people report stomach pain, heartburn, or nausea when they start. These usually fade after a few weeks. If they don’t, talk to your doctor. There’s no need to tolerate side effects that affect your quality of life.
What should you avoid while taking dabigatran?
You don’t need to change your diet like you would with warfarin. No need to avoid leafy greens or limit vitamin K. That’s one big advantage.
But here’s what you do need to avoid:
- Other blood thinners: Don’t take aspirin, ibuprofen, naproxen, or other NSAIDs unless your doctor says it’s safe. These can increase bleeding risk.
- Herbal supplements: St. John’s wort, ginkgo biloba, garlic supplements, and fish oil can interfere with dabigatran. Always tell your pharmacist or doctor what supplements you take.
- Alcohol: Heavy drinking increases bleeding risk. Stick to moderate amounts - no more than one drink a day.
Also, avoid activities with high injury risk - contact sports, rock climbing, or anything where a fall could cause internal bleeding. Wear protective gear when biking or doing yard work. Even minor bumps can lead to serious bruising.

Signs of bleeding - when to call 911
Dabigatran saves lives by preventing clots, but it can also cause bleeding. Most people don’t have problems, but you need to know the warning signs.
Call your doctor right away if you notice:
- Bleeding that won’t stop - like a nosebleed lasting more than 10 minutes
- Unusual bruising, especially large purple patches
- Red or dark brown urine
- Black, tarry stools or blood in stool
- Severe headaches, dizziness, or vision changes (could mean bleeding in the brain)
- Unexplained swelling or pain in joints
If you have a serious fall, head injury, or surgery - even a dental extraction - tell the provider you’re on dabigatran. They may need to pause it temporarily.
What about kidney function?
Dabigatran leaves your body through your kidneys. If your kidneys aren’t working well, the drug can build up and increase bleeding risk.
Your doctor will check your kidney function with a simple blood test before starting and at least once a year after. If your creatinine clearance drops below 30 mL/min, dabigatran may no longer be safe. There are other options in that case.
Dehydration can also affect kidney function. Drink enough water, especially in hot weather or when you’re sick. Don’t wait until you’re thirsty.
What if you need surgery or a dental procedure?
This is one of the most common concerns. You don’t need to stop dabigatran for minor procedures like fillings or biopsies. But for major surgeries - like knee replacement or heart surgery - your doctor will tell you when to stop.
Typically, you stop dabigatran 1 to 3 days before surgery, depending on your kidney health and the procedure’s bleeding risk. Your doctor might use a bridging plan with a short-acting injectable anticoagulant, but that’s rare with dabigatran. Most people don’t need it.
Always carry a medical alert card or app listing your medications. Emergency responders need to know you’re on a blood thinner.
How does dabigatran compare to other blood thinners?
Here’s how dabigatran stacks up against other common anticoagulants:
| Medication | Dosing | Blood Monitoring Needed? | Diet Restrictions? | Reversal Agent Available? |
|---|---|---|---|---|
| Dabigatran (Pradaxa) | Twice daily | No | No | Yes - idarucizumab (Praxbind) |
| Rivaroxaban (Xarelto) | Once daily | No | No | Yes - andexanet alfa |
| Apixaban (Eliquis) | Twice daily | No | No | Yes - andexanet alfa |
| Warfarin (Coumadin) | Once daily | Yes - weekly to monthly | Yes - vitamin K | Yes - vitamin K and fresh frozen plasma |
Dabigatran’s biggest advantage is no regular blood tests. Its biggest downside is that you must take it twice a day. If you forget doses, it’s less effective. Apixaban and rivaroxaban are once-daily options that might be easier for some people.
All of them work well. The best one for you depends on your kidney function, other medications, lifestyle, and personal preference.

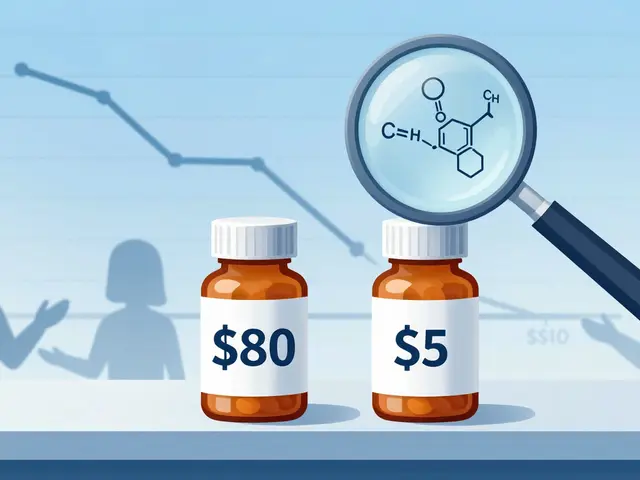
What if you’re worried about cost?
Dabigatran can be expensive without insurance. The brand-name Pradaxa costs over $500 a month in the U.S. But generic dabigatran became available in 2020 and now costs as little as $30 to $60 for a 30-day supply at many pharmacies.
Many drug manufacturers offer patient assistance programs. Check the Pradaxa website or ask your pharmacist. Medicare Part D usually covers it, and some state programs help with co-pays. Don’t skip doses because of cost - talk to your doctor about alternatives or financial help.
Can you take dabigatran long-term?
Yes. Many people take it for years - even for life - especially if they have permanent AFib. It’s safe for long-term use. Studies following patients for over five years show no increase in serious side effects over time.
The key is staying consistent. Missing doses or stopping without medical advice is riskier than any side effect. Keep your pills in a daily pill organizer. Set phone alarms. Ask a family member to remind you if needed.
What happens if you need to stop?
You might need to stop dabigatran if you have major bleeding, severe kidney failure, or need emergency surgery. But stopping for any other reason - like feeling fine or thinking you don’t need it anymore - is dangerous.
Your stroke risk doesn’t disappear just because you feel well. AFib doesn’t always cause symptoms. Clots can still form silently. Stopping dabigatran without replacing it with another anticoagulant can triple your stroke risk in the first 90 days.
If your doctor says it’s time to stop, they’ll give you a plan. Sometimes they switch you to another drug. Other times, they might recommend aspirin or no medication at all - but only if your risk is very low.
Can dabigatran cause weight gain?
No, dabigatran is not linked to weight gain. Unlike some other medications - like certain antidepressants or steroids - it doesn’t affect metabolism or appetite. If you notice unexplained weight gain, it could be due to fluid retention from heart or kidney issues, not the drug itself. Talk to your doctor to find the real cause.
Is dabigatran safe during pregnancy?
Dabigatran is not recommended during pregnancy. It can cross the placenta and may harm the developing baby. If you’re pregnant or planning to become pregnant, your doctor will switch you to heparin injections, which are safer during pregnancy. Always tell your provider if you’re trying to conceive or think you might be pregnant.
Can I drink alcohol while taking dabigatran?
Moderate alcohol is usually okay - one drink per day for women, two for men. But heavy drinking increases your risk of bleeding, especially in the stomach and brain. If you drink regularly, talk to your doctor. They may advise you to cut back or avoid it entirely, especially if you have liver disease or a history of ulcers.
Does dabigatran interact with common painkillers?
Yes. Avoid ibuprofen, naproxen, and other NSAIDs unless your doctor approves them. These drugs can irritate your stomach lining and increase bleeding risk when combined with dabigatran. Acetaminophen (Tylenol) is usually safe for pain or fever. Always check with your pharmacist before taking any new over-the-counter medicine.
How long does it take for dabigatran to leave your system?
Dabigatran has a half-life of about 12 to 17 hours in healthy adults. That means half of it is gone in about a day. Most of it clears from your body within 2 to 3 days. But if your kidneys aren’t working well, it can take longer - up to 5 days. This is why your doctor checks your kidney function before adjusting your dose or stopping the drug.
Next steps: What to do now
If you’re starting dabigatran, here’s your action plan:
- Fill your prescription and get the generic version if available - it’s just as effective.
- Set daily alarms for both doses. Use a pill organizer with morning and evening slots.
- Keep a list of all your medications and supplements to show your doctor at every visit.
- Wear a medical alert bracelet or carry a card that says you’re on an anticoagulant.
- Schedule a follow-up with your doctor in 4 to 6 weeks to check how you’re doing.
Dabigatran is a powerful tool. Used right, it can keep you out of the hospital and help you live longer. But it’s not something you can treat lightly. Stay informed, ask questions, and don’t hesitate to speak up if something feels off. Your life depends on it - and you’re the most important part of your care team.



Jeff Moeller on 20 November 2025, AT 07:45 AM
Dabigatran just feels like a win honestly no more weekly blood draws no weird food rules just take it and go about your life