Picture sitting in your doctor’s office, being told you’re now on Coumadin. Your first thought: Do I need to change my life? Right behind that, you worry about what you can and can’t eat, whether you can have a drink with friends, or if your daily run is suddenly off-limits. Suddenly your blood feels like something dangerous and fragile—a ticking bomb. With Coumadin (that’s warfarin, for the science folks), you’re not alone. Tens of thousands of Australians pop this ‘blood thinner’ every day to dodge clots and strokes. But what makes Coumadin so widespread, and why does it come with so many warnings? Here’s your straight-up guide—no scare tactics, just hard facts, real stories, and plenty of insider tips straight from Perth, where health advice is as no-nonsense as the weather.
Why Doctors Prescribe Coumadin
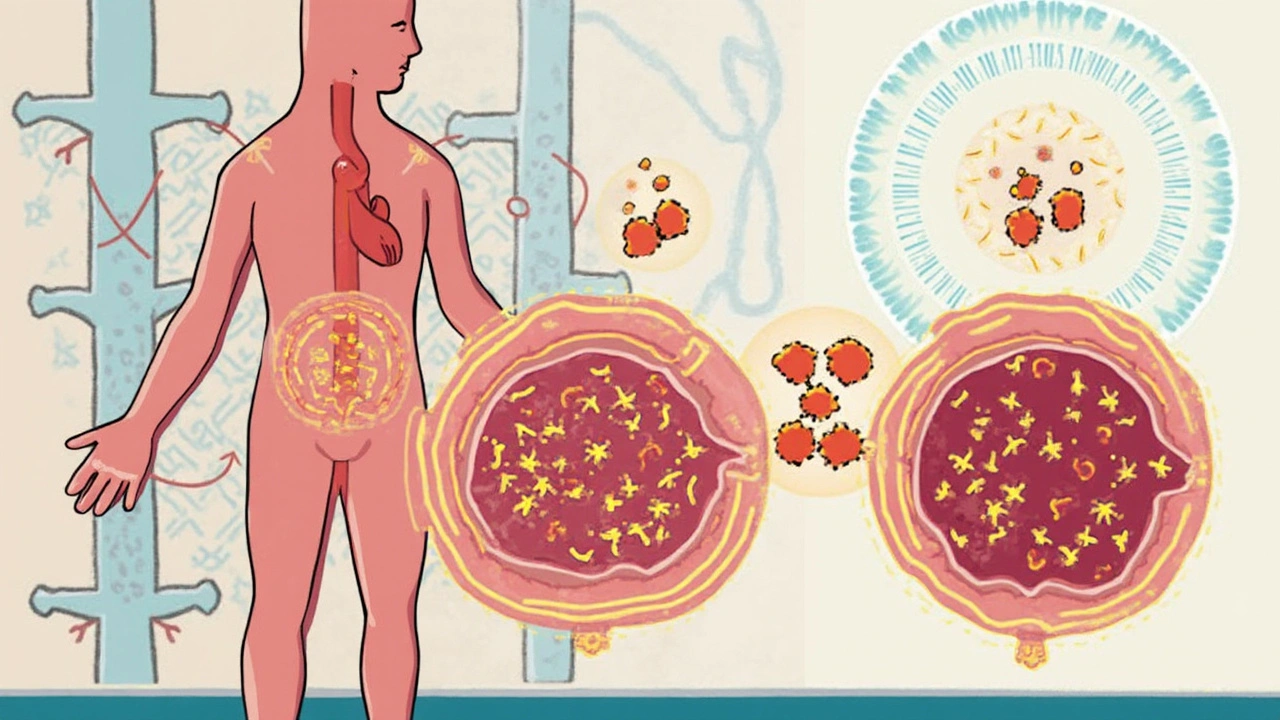
Coumadin, the brand name for warfarin, isn’t your average pill. It’s the most prescribed anticoagulant in Australia and around the globe, especially for people at high risk for blood clots—that means anyone with deep vein thrombosis (DVT), pulmonary embolism, atrial fibrillation (a wonky heartbeat), certain heart valve issues, or even folks who’ve had major surgeries. The reason is simple: Coumadin keeps your blood from clotting where it shouldn’t. Think of it as insurance against strokes, heart attacks, and sometimes even death.
So how exactly does this tiny pill pull off such a tricky job? Coumadin works by blocking the action of vitamin K in your liver. Vitamin K helps your body make certain clotting factors. No vitamin K means fewer of these factors, so your blood flows a bit more freely—just enough to prevent clots, but not so much you’re in danger of bleeding out from a paper cut. That sweet spot is everything. Get it wrong and blood clots could form; tip the scales the other way and you risk serious bleeding.
Not everyone gets Coumadin straight away. Doctors usually try other drugs for short-term clot prevention because Coumadin can be tricky—interactions, diet, and genetics all play a part. But when you need long-term anticoagulation, or newer drugs aren’t an option, Coumadin still gets the green light. Its track record is rock solid—just look at the stats: In 2023, about 80,000 Australians filled out at least one warfarin script, according to national PBS data.
Now, just because Coumadin is everywhere doesn’t mean you can take it lightly. Regular monitoring is non-negotiable. People on Coumadin check something called INR (International Normalized Ratio) often. That’s a measure of how long it takes your blood to clot, with a normal range being roughly between 2 and 3 for most cases. Go too low, risk clots; too high, risk bleeding.
Doctors also carefully check if you’re a good candidate: do you have falls risk? Are you good at remembering pills? Is your kidney or liver up to the job? If they go ahead, they’ll brief you on the quirks and rules of Coumadin, especially the role of vitamin K and all the food, drink, and drug interactions. You’re in for some life adjustments, but none of them are impossible.
How To Take Coumadin—and Not Lose Your Mind
No sugarcoating here—life on Coumadin means being more aware, but you absolutely can still live well. First off, doses vary a lot. Some folks take a tiny 1 mg, others go up to 10 mg or have to adjust almost every week. Your perfect dose depends on your age, kidney function, diet, other medications, and sometimes genetics (yes, some people are ‘warfarin sensitive’ and need less). Doctors usually start low and titrate up, checking your INR every few days at the start, then maybe once a month when you’re stable.
Consistency is everything. Take Coumadin at the same time each day—usually around dinner, but if you’re a night owl or early riser, just keep it steady. Don’t skip doses, and don’t double up if you miss one. Those swings show up in your next INR and mess with your clotting time.
Keep a list—on paper, on your fridge, wherever—of everything you put in your body. That means vitamins, herbal teas, supplements, painkillers, even some antibiotics. When you start or stop a medicine, or even binge on kale for a week, your INR may shift. No drama, just let your doctor know and get checked if anything feels weird.
Your diet doesn’t have to be boring, you just need balance. Suddenly going from zero greens to a plate of broccoli for every meal? Your INR may drop too low, and you risk a clot. On the other hand, cutting out all leafy greens cold turkey can bump your INR up and tip you toward bleeding. The trick is, enjoy your veggies, just don’t go wild with the changes week to week. Here’s a quick cheat sheet of vitamin K in common foods:
| Food | Vitamin K (mcg per serving) |
|---|---|
| Boiled spinach (1 cup) | 900 |
| Broccoli (1/2 cup) | 90 |
| Iceberg lettuce (1 cup) | 17 |
| Avocado (whole) | 30 |
| Egg (boiled) | 0.3 |
Besides food, alcohol’s another biggie. No, you don’t have to be a monk, but binge drinking sends your INR haywire. One beer or wine per day, if that’s your groove, is usually fine. Just be upfront with your doctor if you occasionally celebrate hard.
Remember, Coumadin takes time to kick in—a couple of days, minimum. If you’re starting, your doctor might cover you with heparin shots until your INR is safe. If you’re stopping, the opposite: don’t quit cold unless the doc says so. All those rules sound strict, but after the first month, most people settle into a rhythm.
Life Hacks for Living Well on Coumadin
So you’re past the scary part. You’ve started on Coumadin and survived your first couple of INR checks. Now comes the part where this drug sneaks into all corners of your life. But hey, you can totally handle it with a bit of planning—and maybe some humor.
INR checks can be a pain, so make them fit your routine. Some pharmacies in Australia, even in Perth suburbs, now offer finger-prick INR testing on the spot—no massive hospital queues. Or, if you’re tech-savvy and your doctor approves, at-home INR testing kits – like the CoaguChek – are available (though these aren’t cheap and not always covered by Medicare). Whichever way, schedule tests for the same day each month to keep things simple.
Traveling? Always pack extra tablets and a copy of your latest INR readings. Most countries know warfarin, but border security may ask, so keep your prescription handy. Flying isn’t off-limits, but you do need to move often on long flights to avoid leg clots. Wear compression socks and drink water.
Physical activity is totally okay—actually, it’s crucial. Just know your risk. High-contact sports aren’t the best idea. Cycling is fine; MMA, probably not. Tell your trainer or gym buddies—if you ever take a tumble and start bruising easily, it might be a Coumadin thing and worth a quick check. If your gums bleed while brushing or you notice dark stools, that’s a flag for your care team.
Tattoo lovers or the ink-curious, a little heads-up: Coumadin doesn’t mean you can’t get tattoos or piercings, but you’ll need your INR in-range and let your artist or piercer know. Same goes for dental work—let your dentist know early so they can plan around your meds.
Personal story from my mate Liam in Fremantle: he did his first marathon on Coumadin, only after gradual training and clearing it with his doctor. He kept his INR in check and always carried his medic-alert ID on his shoe. No issues, just lots of pasta and finish-line bragging rights.
Speaking of IDs, medic alert bracelets or wallet cards are key if you’re on Coumadin. If something happens and you’re knocked out (let’s hope not), first responders will want to know your blood might not clot the usual way.
Don’t forget to check in with your care team. Check-ups and blood draws are annoying, but they’re your safety net. If you get the flu, have vomiting, diarrhea, or a new prescription, or even drop a lot of weight, your warfarin dose might need changing. Ignore your body at your own risk.
The Most Common Side Effects and Red Flags
Warfarin’s rep for being dangerous isn’t pulled out of thin air. The balance it strikes is delicate—and side effects, if you’re not paying attention, can creep up. Top of the list is bleeding. Most people will have a bruise or two that comes from nowhere—it’s a Coumadin classic and usually not a big deal. But significant bleeding means anything from long, heavy nosebleeds or gums that won’t quit, to blood in your urine, black or tarry stools, or coughing up anything bloody. Women might spot heavier periods.
If you whack your head or hit your stomach hard, get checked—internal bleeding can be slow and silent. Coumadin’s not forgiving if you let those signs slide. Rarely, people get Coumadin skin necrosis: weird purple skin patches that pop up in the first few days of treatment. It’s rare, but you’ll know if you see it—call your doctor straight away.
Some meds crank up your Coumadin levels; others tank them. Antibiotics like Bactrim and metronidazole, antifungals, even paracetamol in big doses—all raise INR. On the other hand, hard-core sleep aids or vitamin K-rich herbal supplements send your INR crashing down. Your pharmacist is your wingman here; double-check everything.
Alcohol, as mentioned, is a wildcard—keep tabs on it. Your liver does all the heavy lifting with Coumadin, and those rounds at your local pub in Northbridge can make it work overtime.
Sometimes, weird stuff happens—like hair falling out (usually mild and short-term), or feeling a weird metallic taste. No need for panic, but let your doctor know.
A huge tip: injuries on Coumadin can look a bit scary—think big colorful bruises. But if they get hot, tender, or start spreading, or if you spot unexplained swelling (especially in one leg—could be a clot), that’s a hospital job. Don’t mess around.
Check out these real-world stats from a case review at Royal Perth Hospital (2022 data):
| INR Range | Clinical Outcome (per 100 people per year) |
|---|---|
| Below 2.0 | 5 DVT/PE events, 1 major bleed |
| 2 - 3 | 1 DVT/PE event, 1.5 major bleeds |
| Above 4.0 | 0 DVT/PE, 6 major bleeds |
Notice how too low risks clots, and too high risks bleeding disasters. That’s why that sweet INR spot is gospel.

Switching or Stopping: What Happens Next?
At some point, you and your doctor might talk about swapping Coumadin for a newer drug, or maybe stopping anticoagulation altogether. ‘NOACs/DOACs’—the newer ones like Eliquis, Xarelto, Pradaxa—don’t need regular blood tests and have fewer food interactions. That said, they aren’t always suitable, especially if you have new mechanical heart valves or kidney issues. Warfarin still holds the fort for a lot of Aussies, especially older folks used to their routine.
If you do need to stop Coumadin (maybe your surgery’s ahead, or you’ve had a few nasty bleeds), you can’t just stop cold. Your doctor will taper your dose, check your INR, and sometimes bridge with another short-acting blood thinner for safety. Going in for surgery or dental extractions? Surgeons often tell you to hold Coumadin for a couple of days pre-op, then restart once it’s safe.
Be aware: Coumadin can stay in your system a few days after stopping. It takes your body another week (sometimes longer) to get back to its old clotting habits. That “bridge time” is risky for both bleeding and clotting, so only do it with doctor’s orders. Sometimes, for short procedures, they don’t stop Coumadin at all—they just make local adjustments.
If you ever need a reversal for major bleeding, doctors in Australia use vitamin K (sometimes IV, sometimes oral), and, in an emergency, use a clotting factor concentrate or fresh frozen plasma. This isn’t stuff to DIY—if you feel off, get professional help.
It’s a bit like driving an old stick-shift ute—works just fine if you’re careful and follow the rules, but you have to pay attention, know when to shift, and occasionally fix a glitch. Coumadin isn’t scary once you really get how it works. Most people go years with zero drama, with a little planning and some sharp instincts.





Kristin Violette on 22 May 2025, AT 17:44 PM
When you first get your INR reading, think of it as the pharmacodynamic fingerprint of your warfarin dose – it tells you whether you’re cruising in the therapeutic window or veering off into dangerous territory. Consistency is king: take your pill at the same clock‑time each day, ideally with a small snack to smooth absorption. Keep a simple log of any greens, supplements, or antibiotics – even a weekend binge on kale can shift your INR by a full point. If the numbers drift, contact your clinic before you adjust anything yourself; the lab can help you fine‑tune the dose without courting a bleed. Remember, the goal isn’t perfection, just a stable range that keeps clots at bay while sparing you from bruises.