Medication Side Effect Timeline Calculator
Predict Your Side Effect Timeline
Enter your details to get an estimated timeline of when side effects might appear for your medication.
When you start a new medication, you might wonder: when will the side effects show up? It’s not just about whether they’ll happen-it’s about when. Knowing the timeline can mean the difference between panicking over a normal adjustment and spotting something dangerous early. Some reactions hit within minutes. Others creep in over weeks. And if you don’t know what’s normal, you might stop a life-saving drug-or ignore a life-threatening one.
Immediate Reactions: Minutes to One Hour
If you feel dizzy, break out in hives, or can’t breathe right after swallowing a pill, don’t wait. These are immediate reactions, and they’re serious. Anaphylaxis, the most dangerous type, usually strikes within 15 to 30 minutes. Studies tracking over 1,200 emergency cases found that nearly 70% of penicillin-related anaphylaxis cases began within 15 minutes of dosing. Other quick reactions include sudden swelling of the lips or tongue, wheezing, or a rapid drop in blood pressure.This isn’t rare. About 1 in 50 people will have some form of immediate allergic reaction to a medication they’ve never taken before. That’s why doctors often ask you to wait in the clinic after your first dose of certain antibiotics or vaccines. It’s not bureaucracy-it’s safety. If you’ve had a severe reaction before, you’ll be given an epinephrine auto-injector and told to carry it everywhere. No exceptions.
Early Delayed Reactions: 1 to 72 Hours
Not all side effects come screaming in. Many show up quietly between one and three days later. This window covers the bulk of common drug allergies. Think of it as your body’s delayed response-like a slow-burning fuse.Drug-induced rashes, fever, joint pain, and mild liver enzyme spikes often appear here. For example, if you start amoxicillin and get a red, blotchy rash around day two or three, it’s likely not an allergy-it’s a common non-allergic reaction. But if the rash spreads, blisters, or is accompanied by fever and swollen lymph nodes, it could be something more serious like DRESS syndrome, which we’ll get to later.
According to clinical data, 92% of drug allergy symptoms that aren’t anaphylactic show up within this 72-hour window. That’s why your pharmacist tells you to watch the first few days closely. If you’re on a new medication and start feeling off-itchy, nauseous, or just generally “wrong”-don’t brush it off. Log it. Note the time. Track the pattern. This is your first line of defense.
Delayed Reactions: 4 Days to 8 Weeks
This is where things get tricky. Many people assume if they’ve made it past the first week without issues, they’re safe. Not true. Some of the most dangerous side effects take weeks to emerge.Maculopapular rashes-the most common drug-induced skin reaction-typically appear between days 4 and 14. For antibiotics like amoxicillin or sulfonamides, the median onset is day 8. That’s why doctors often tell patients to keep taking the medicine for a few days even if they develop a mild rash. Sometimes, it’s just your body adjusting. But if it worsens, you need to stop.
Then there’s DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms). This rare but deadly reaction usually starts around week two or three. It begins with a fever and rash, then can lead to liver failure, kidney damage, or even heart inflammation. The median onset for anticonvulsants like carbamazepine or phenytoin is 28 days. In one study of 317 patients, 87% of DRESS cases appeared between days 14 and 42. Missing this window can be fatal.
Other delayed reactions include drug-induced lupus (from medications like hydralazine or procainamide), which can take months to develop but often shows early signs like joint pain and fatigue after 4-6 weeks. Or thyroid dysfunction from amiodarone-side effects that don’t show up until you’ve been on it for three months.

Chronic Reactions: Beyond 8 Weeks
Some side effects don’t just delay-they build up. Like rust on a pipe, damage accumulates slowly. These reactions are easy to miss because they’re subtle and blamed on aging, stress, or other conditions.Statins like atorvastatin can cause muscle pain or weakness within 7-10 days for 5-10% of users. But for others, it takes months. The same goes for long-term use of proton pump inhibitors (PPIs) like omeprazole. After six months, you might develop low magnesium levels, increasing your risk of irregular heartbeat. After two years, you could be at higher risk for bone fractures.
One of the most insidious examples is amiodarone, used for heart rhythm problems. It can cause lung scarring (interstitial lung disease) after 6 to 12 months. Symptoms? Shortness of breath, dry cough, fatigue. Many patients think it’s just getting older-until their lungs are permanently damaged.
These aren’t accidents. They’re predictable. That’s why doctors monitor liver enzymes, kidney function, and thyroid levels for patients on long-term meds. If you’ve been on a drug for more than three months and feel “off,” ask: Could this be the medication?
What Makes the Timeline Different for Everyone?
Why does one person get a rash on day 3 and another never has a problem? It’s not luck. It’s biology.Dosage matters. Higher doses speed up side effects. In one study, 82% of dose-dependent reactions appeared within 24 hours-compared to just 47% at standard doses.
Age changes everything. People over 65 process drugs 2.3 days slower on average. That means side effects hit later and last longer. A 70-year-old on a new blood pressure pill might not feel dizzy until day 5, while a 30-year-old felt it by day 2.
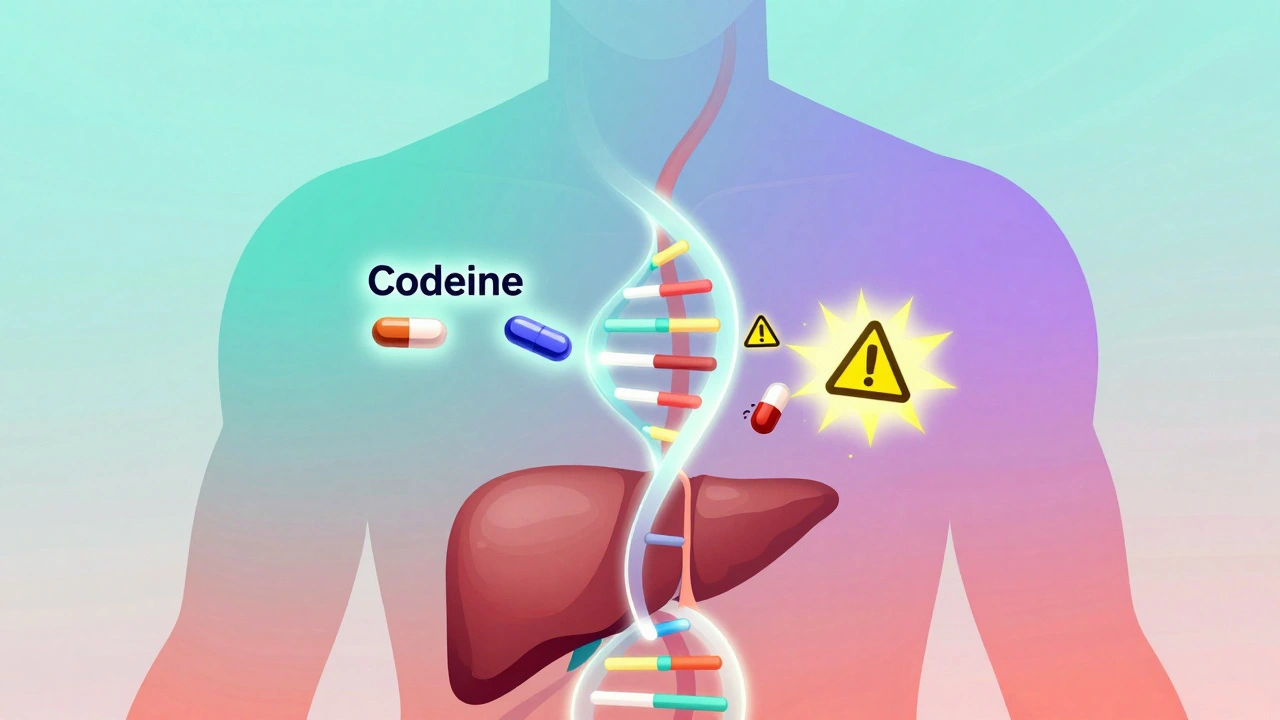
Genes play a huge role. If you carry the HLA-B*57:01 gene, taking the HIV drug abacavir will trigger a life-threatening reaction within 48 hours-every time. That’s why genetic testing is now standard before prescribing this drug. Same goes for CYP2C19 gene variants: they can make clopidogrel (a blood thinner) ineffective or cause side effects to appear 2.7 days earlier than normal.
Other health conditions matter too. If you have kidney disease, drugs that are cleared through your kidneys build up faster. If you have an autoimmune disorder, your immune system is already on high alert-so it reacts quicker to foreign substances. One study showed these patients develop side effects 37% faster than others.
Even switching from brand to generic can change the timeline. About 23% of patients report side effects appearing sooner or differently when they switch, often because of different fillers or coatings in the pill. It’s not the active ingredient-it’s the extras.

What You Should Do: A Practical Timeline Checklist
You don’t need to be a doctor to protect yourself. Here’s what to do, by the clock:- First hour: Stay where you can get help. Watch for swelling, trouble breathing, or dizziness. If any of these happen, call emergency services.
- Days 1-7: Check daily. Note any rash, nausea, headache, or unusual fatigue. Keep a simple log: “Day 3: mild itching after taking pill.”
- Weeks 2-4: Especially critical for antidepressants, anticonvulsants, and blood pressure meds. Side effects like emotional numbness, muscle pain, or liver issues often peak here. Schedule your follow-up appointment. Don’t skip it.
- Weeks 5-8: Still watch for rashes, fever, or swollen glands. These could be signs of DRESS or other delayed reactions. Don’t assume you’re safe just because you’ve made it this far.
- Months 3+: If you’re on long-term meds, ask your doctor about routine blood tests. Ask: “What side effects should I watch for after six months?”
And here’s the golden rule: Write it down. A 2021 study found that patients who tracked symptoms with exact timing were 63% more likely to correctly identify a medication side effect versus a cold, flu, or stress reaction. That’s not a small edge-it’s the difference between getting the right treatment and being misdiagnosed.
When to Call Your Doctor (And When to Go to the ER)
Not every side effect needs an emergency room. But some do.Go to the ER if you have:
- Difficulty breathing or tightness in your throat
- Sudden swelling of the face, lips, or tongue
- Severe dizziness or fainting
- A rash with blistering, peeling skin, or sores in your mouth
- High fever (over 38.5°C) with rash and swollen lymph nodes
Call your doctor within 24-48 hours if you have:
- A spreading rash that itches or burns
- Yellowing skin or eyes (sign of liver stress)
- Unexplained muscle pain or weakness
- Persistent nausea, vomiting, or dark urine
- New mood changes, confusion, or memory problems
For mild nausea, headache, or drowsiness that fades after a few days? That’s often your body adjusting. But if it doesn’t improve by day 7, talk to your doctor. Don’t wait.
The Future: Predicting Side Effects Before They Happen
The good news? We’re getting better at stopping side effects before they start.Genetic testing is now part of standard care for certain drugs. Hospitals in major cities use AI tools to predict your risk based on your genes, age, kidney function, and other meds you take. One system developed by Mayo Clinic predicts side effect timing with 84% accuracy using just 12 data points.
Apps that track symptoms and remind you to log reactions are cutting emergency visits by 32%. In Australia, some pharmacies now offer free side effect tracking tools with your prescription.
This isn’t science fiction. It’s here. And it’s saving lives.
Knowing when side effects appear isn’t just helpful-it’s essential. It turns fear into control. Confusion into clarity. And in many cases, it turns a near-disaster into a simple adjustment.
How soon after taking a new medication can side effects start?
Side effects can start as quickly as minutes after taking a medication-especially with allergic reactions like anaphylaxis. Most common side effects appear within the first 72 hours. But some, like certain rashes or organ damage, may take days to weeks. For example, DRESS syndrome typically shows up 2 to 8 weeks after starting the drug. Always monitor your body closely during the first eight weeks of any new medication.
Can side effects appear after months or years of taking a medication?
Yes. Some medications cause damage that builds up over time. For instance, amiodarone can cause lung scarring after 6-12 months. Long-term use of proton pump inhibitors may lead to low magnesium or bone loss after two years. Even statins can cause muscle damage that develops slowly. These aren’t immediate reactions-they’re chronic ones. Regular check-ups and blood tests are key if you’re on long-term meds.
Are side effects more likely if I’m older?
Yes. As you age, your liver and kidneys process drugs more slowly. This means medications stay in your system longer, increasing the chance of side effects-and delaying when they appear. People over 65 often experience side effects 2.3 days later than younger adults. That’s why older patients need lower doses and closer monitoring.
Can switching from brand to generic medication change when side effects appear?
Yes. While the active ingredient is the same, generics can use different fillers, coatings, or binding agents. These can affect how quickly the drug is absorbed. About 23% of patients report side effects appearing sooner or differently after switching. If you notice a change in how you feel after switching, tell your doctor. It’s not all in your head-it’s chemistry.
Should I stop taking my medication if I get a side effect?
Don’t stop without talking to your doctor. Some side effects, like mild nausea or drowsiness, fade as your body adjusts. Stopping suddenly can be dangerous-for example, stopping antidepressants or blood pressure meds can cause withdrawal or rebound effects. But if you have signs of a severe reaction-trouble breathing, swelling, blistering skin-stop the medication and seek emergency help immediately.
Is there a way to predict if I’ll have side effects before starting a new drug?
Yes, increasingly so. Genetic testing can now predict your risk for severe reactions to certain drugs-like abacavir or carbamazepine. Some hospitals use AI tools that analyze your age, medical history, other medications, and genes to estimate your personal risk and likely timeline for side effects. While not yet available everywhere, this is becoming standard in major healthcare systems.



Ayodeji Williams on 8 January 2026, AT 10:30 AM
Bro i took amoxicillin and got a rash on day 2 😅 thought i was dying but it was just my body being dramatic. Now i log everything like a mad scientist. 📝