Beta-Blocker + CCB Safety Checker
Patient Assessment
Enter patient parameters and click "Check Safety" to see if this combination is safe.
When doctors combine beta-blockers and calcium channel blockers, they’re not just adding two pills together-they’re mixing two powerful forces that slow down the heart in different ways. For some patients, this combo works wonders. For others, it can be dangerous. The key isn’t just knowing the names of the drugs, but understanding which calcium channel blocker you’re using and who you’re giving it to.
How These Drugs Work-And Why They’re Combined
Beta-blockers like metoprolol, atenolol, and propranolol reduce heart rate and force of contraction by blocking adrenaline’s effects. Calcium channel blockers, on the other hand, stop calcium from entering heart and blood vessel cells. This relaxes arteries and lowers blood pressure. The idea behind combining them is simple: if one drug doesn’t fully control your blood pressure or chest pain, adding another with a different mechanism might help.
This approach isn’t new. Back in the 1980s, guidelines started recognizing dual therapy for hard-to-treat high blood pressure. Today, it’s still used-but only for specific cases. The 2018 European Society of Cardiology guidelines say this combo is acceptable for patients with hypertension and angina who haven’t responded to single drugs. But they’re very clear: avoid verapamil or diltiazem with beta-blockers if you have any heart rhythm issues.
The Big Divide: Dihydropyridines vs. Non-Dihydropyridines
Not all calcium channel blockers are the same. There are two major types, and mixing them with beta-blockers has wildly different outcomes.
Dihydropyridines-like amlodipine, nifedipine, and felodipine-mostly act on blood vessels. They dilate arteries, lowering blood pressure without strongly slowing the heart. When paired with a beta-blocker, this combo is generally safe and effective. Studies show it reduces heart attacks and strokes better than many other dual therapies. In fact, a 2023 study of nearly 19,000 Chinese patients found those on metoprolol + amlodipine had a 17% lower risk of major heart events than those on other combinations.
Non-dihydropyridines-verapamil and diltiazem-are different. They hit the heart hard. They slow the electrical signals that control heartbeat and reduce how strongly the heart pumps. When you add a beta-blocker to these, you’re doubling down on heart slowdown. The result? Dangerous drops in heart rate, prolonged PR intervals on ECG, and even heart block.
A 2023 NIH study found that 10-15% of patients on verapamil + beta-blocker developed serious bradycardia or heart block. That’s not rare-it’s common enough that doctors should expect it. In elderly patients, the risk of needing a pacemaker jumps 3.2 times compared to those on beta-blocker + amlodipine.
Who Should Never Get This Combo?
Some patients shouldn’t even be considered for this treatment. The risks are too high.
- Patients with sinus node dysfunction (sick sinus syndrome)
- Those with second- or third-degree AV block
- Anyone with a PR interval longer than 200 milliseconds on ECG
- People with heart failure and reduced ejection fraction (HFrEF)
- Older adults over 75 with unknown conduction issues
One cardiologist on Reddit shared a heartbreaking case: an 82-year-old man on metoprolol was given verapamil for high blood pressure. His PR interval was borderline-just under 200ms. Within weeks, he went into complete heart block. He needed an emergency pacemaker. That’s not an outlier. It’s a warning.
The European Medicines Agency now requires doctors to check ejection fraction before starting this combo. The FDA added a boxed warning for verapamil + beta-blocker use in patients with conduction problems. These aren’t bureaucratic footnotes-they’re life-saving alerts.
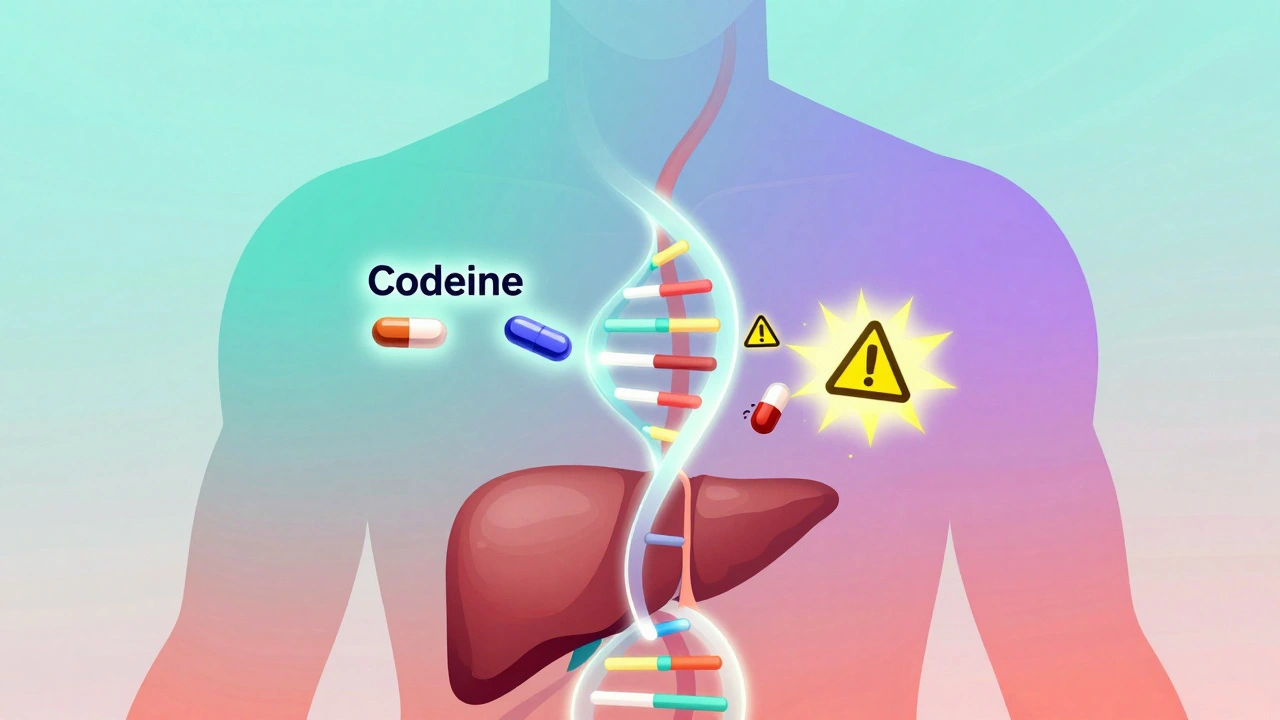
What Happens in the Body When You Mix Them?
The cardiac effects aren’t theoretical-they show up in measurable numbers.
- Resting heart rate can drop by 25-35 beats per minute with verapamil + beta-blocker, compared to 15-25 with either alone.
- PR interval (the time it takes for the heart’s electrical signal to travel from atria to ventricles) can stretch by 40-80 milliseconds-enough to cause dangerous delays.
- In patients with existing heart weakness, left ventricular ejection fraction can fall by 15-25% with verapamil + beta-blocker, versus 5-8% with one drug alone.
- Left ventricular end-diastolic pressure rises in heart failure patients on beta-blocker + nifedipine, making the heart work harder to fill.
These aren’t just lab values. They’re signs of strain. A slow heart rate might feel like fatigue. A prolonged PR interval might cause dizziness. A drop in ejection fraction might lead to shortness of breath. All of it can escalate quickly.
Why Some Doctors Still Use Verapamil + Beta-Blocker
It’s not that doctors are ignoring the risks. In some cases, the benefits outweigh them.
For patients with angina who can’t tolerate other drugs, verapamil + beta-blocker can improve exercise tolerance by 90-120 seconds. That’s meaningful for someone who can’t walk up stairs without chest pain. But this benefit only applies to patients with normal heart function-ejection fraction above 50%, no conduction delays.
Even then, the trade-offs are steep. A 2020 study found 18.7% of patients on verapamil + beta-blocker stopped the combo due to side effects like dizziness, fatigue, or swelling. With amlodipine + beta-blocker, that number was just 8.1%. That’s more than double the dropout rate.
And then there’s the swelling. Beta-blocker + dihydropyridine combos cause peripheral edema (ankle swelling) in about 22% of patients. That’s higher than other dual therapies. But it’s usually mild and manageable with a lower dose or diuretic. It’s not life-threatening-unlike heart block.

How to Use This Combo Safely
If your doctor considers this combination, here’s what should happen before and after:
- Get a baseline ECG. Check the PR interval. If it’s over 200ms, don’t proceed.
- Have an echocardiogram. Measure ejection fraction. If it’s below 45%, avoid non-dihydropyridine CCBs.
- Start low, go slow. Begin with half the usual dose of each drug.
- Monitor heart rate daily for the first month. If it drops below 50 bpm, call your doctor.
- Check for swelling, dizziness, or unusual fatigue. These aren’t just side effects-they’re warning signs.
Tools like the European Society of Cardiology’s online bradycardia risk calculator (validated on over 4,500 patients) help predict who’s at risk. In hospitals like Kaiser Permanente, where standardized protocols were introduced in 2020, adverse events dropped by 44%.
What the Experts Say
Dr. Giuseppe Mancia, lead author of the 2022 AHA Hypertension study, says beta-blockers are still valuable-especially for patients with resting heart rates above 80 bpm. But he’s clear: if you need a calcium channel blocker, pick amlodipine, not verapamil.
Dr. Robert M. Carey, former president of the American Heart Association, echoes this: “Beta-blockers and calcium channel blockers can work well together-but only if you pick the right calcium blocker.”
Dr. Franz H. Messerli’s 2017 analysis showed the combo increases ankle swelling by 35% compared to other dual therapies. That’s a nuisance, not a crisis. But when you add in the risk of heart block, the cost-benefit shifts dramatically.
The bottom line? If you’re on a beta-blocker and your doctor suggests adding a calcium channel blocker, ask: “Is this amlodipine or verapamil?” If it’s verapamil, ask why. And if you’re over 65, ask for an ECG first.
The Future of This Combo
Use of beta-blocker + verapamil is declining. In the U.S., only 12% of dual therapy prescriptions for hypertension include this combo. In China, it’s higher-22%-but even there, guidelines are tightening.
GlobalData predicts beta-blocker + dihydropyridine prescriptions will grow 5.7% annually through 2028. Why? Aging populations, rising hypertension, and smarter prescribing. The trend is clear: we’re moving toward safer combinations, not riskier ones.
The European Society of Hypertension is developing a new risk stratification tool expected to launch in 2024. It will help doctors decide, in seconds, whether a patient is safe for this combo-or if they need a different path.
For now, the message is simple: don’t assume two good drugs make a better combo. Sometimes, they make a dangerous one.
Can I take beta-blockers and calcium channel blockers together?
Yes-but only under strict conditions. The combo is safe with dihydropyridine CCBs like amlodipine, especially for patients with high blood pressure and angina. It’s dangerous with non-dihydropyridines like verapamil or diltiazem, particularly if you have a slow heart rate, conduction problems, or heart failure. Always get an ECG and echocardiogram before starting.
What’s the difference between amlodipine and verapamil?
Amlodipine mainly relaxes blood vessels, lowering blood pressure without strongly affecting heart rhythm. Verapamil directly slows the heart’s electrical system and reduces pumping strength. When combined with a beta-blocker, amlodipine is generally safe; verapamil can cause dangerous heart block or low blood pressure.
Is this combo safe for older adults?
It’s risky. Over 75% of patients over 75 have undiagnosed conduction abnormalities. Verapamil + beta-blocker in this group increases pacemaker need by over 3 times. Amlodipine + beta-blocker is safer, but still requires close monitoring. Never start this combo in elderly patients without an ECG and echocardiogram.
What are the signs this combo is causing problems?
Watch for: heart rate below 50 bpm, dizziness or fainting, unusual fatigue, swelling in ankles, or shortness of breath. If you’re on verapamil + beta-blocker and feel your heart skipping or slowing, seek help immediately. These aren’t normal side effects-they’re red flags.
Why do some doctors still prescribe verapamil with beta-blockers?
In rare cases, for patients with severe angina who don’t respond to other drugs, the combo can improve exercise tolerance. But this is only considered when the patient has normal heart function, no conduction delays, and no history of heart failure. Most doctors avoid it now because safer alternatives exist.
How often should I get checked if I’m on this combo?
In the first month, check your heart rate daily and see your doctor weekly. After that, monthly ECGs and blood pressure checks are recommended. If you’re on verapamil, get an echocardiogram every 6 months. Any drop in heart rate below 50 or rise in PR interval beyond 200ms means you need a reassessment.




Ryan Barr on 7 January 2026, AT 10:41 AM
Amlodipine + beta-blocker is the only combo that doesn't turn your heart into a slow-motion slideshow.Verapamil? That's just cardiac Russian roulette.