Medication Temperature Risk Calculator
How It Works
Enter your shipment details to calculate temperature risks. This tool simulates how temperature deviations affect medication safety based on WHO and FDA guidelines.
• Enter drug type and shipment duration • Paste temperature log data (CSV format) • Results show risk level and potential consequences
Paste data in format: timestamp,temperature (e.g., 08:00,4.2)
Risk Assessment
Temperature Thresholds
Key Findings
When you pick up your prescription, you assume the medicine inside that bottle is safe, effective, and exactly what your doctor ordered. But what if the journey it took to get there - from factory to pharmacy - was broken? Pharmaceutical supply chain quality isn’t just a behind-the-scenes logistics issue. It’s the difference between life and death for millions of patients worldwide.
What’s at Stake When the Supply Chain Fails
The global pharmaceutical supply chain moves billions of doses every year across 180 countries. It’s not a simple pipeline. It’s a fragile web of manufacturers, distributors, warehouses, and delivery systems - each step requiring precise control. A single temperature spike, a counterfeit vial, or a delayed shipment can derail treatment for someone with cancer, diabetes, or epilepsy. According to the WHO, over 30% of medicines in low-income countries are substandard or falsified. Even in the U.S., where regulations are tighter, drug shortages spiked 300% in the first six months of the COVID-19 pandemic. That wasn’t just inconvenience - it was danger. Patients missed critical infusions. Doctors had to swap insulin brands mid-treatment. Nurses rationed epinephrine for allergic reactions. One patient with multiple sclerosis shared on RateMDs: “My Tysabri infusions were delayed 17 days. Two new brain lesions showed up on my MRI.” That’s not an outlier. The American Hospital Association found 68% of hospitals made medication substitutions during shortages - and 29% of those led to adverse reactions.Why the Supply Chain Is So Fragile
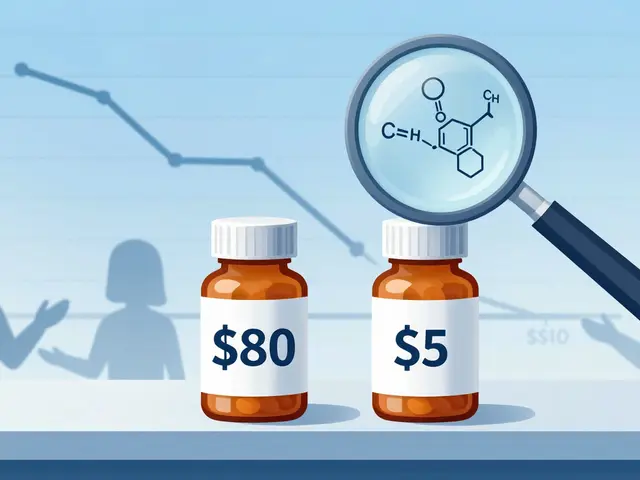
Unlike buying groceries or electronics, pharmaceuticals can’t tolerate mistakes. Seventy-two percent of biologic drugs need constant refrigeration between 2°C and 8°C. Fifteen percent require ultra-cold storage below -60°C - colder than Antarctic winter. One hour outside that range, and the drug loses potency. Sometimes, it becomes toxic. Then there’s the manufacturing bottleneck. Over 78% of active pharmaceutical ingredients (APIs) - the core chemical components of drugs - come from just two countries: China and India. A single factory shutdown, a trade dispute, or a natural disaster like Hurricane Helene in 2024 can ripple across the entire system. When Baxter’s North Carolina plant went offline, more than 80% of U.S. hospitals faced critical shortages. And it’s not just weather or politics. Cyberattacks hit hard. In 2024, a software failure from CrowdStrike knocked out 759 hospitals, halting prescriptions, lab orders, and IV pumps. Patients waited. Treatments were canceled. Staff scrambled.Regulations That Should Work - But Don’t Always
The FDA’s Drug Supply Chain Security Act (DSCSA) was supposed to fix this. By late 2023, every prescription drug had to carry a 2D barcode for full traceability. By November 2025, every transaction must be tracked electronically. Sounds solid, right? The problem? Implementation is uneven. Hospitals report a 14- to 18-month learning curve just to get staff trained. Integrating old systems with new serialization tech is a nightmare - 76% of facilities struggle with it. And while big companies like Pfizer have top-rated protocols, generic manufacturers often cut corners. Their documentation scores average 3.2 out of 5. Even with better tracking, the system still fails at the last mile. In rural areas, 32% of deliveries lose temperature control because delivery trucks aren’t equipped. A vaccine or insulin sitting in a non-refrigerated van for hours might look fine - but it’s already compromised.
Technology Is Helping - But Not Enough
Blockchain adoption has jumped 37% since 2020. Real-time temperature monitors now cover 68% of high-value shipments, cutting temperature excursions by 42%. AI-driven demand forecasting is expected to reduce shortages by 35% by 2027. These aren’t sci-fi ideas - they’re being used now. But cost is a barrier. Building a single cold-chain distribution center runs $2.8 million. Hospitals spend $450,000 and eight months just to install track-and-trace systems. Many small pharmacies and clinics can’t afford it. Meanwhile, the global market for pharmaceutical logistics is worth $1.5 trillion - yet only 12 major distributors control 67% of it. That concentration makes the system more vulnerable, not less. And cybersecurity? A 2023 Censinet report found 74% of healthcare cyberattacks came from third-party vendors - suppliers, freight companies, software providers. One weak link can bring down the whole chain.Who Pays the Price?
It’s not the executives or the logistics managers. It’s the patient. A diabetic waiting for insulin because a shipment got stuck in customs. A child with asthma who can’t get albuterol because a factory in India shut down for inspection. A cancer patient whose targeted therapy was replaced with a less effective generic - and whose tumor started growing again. In 2024, medication errors tied to supply chain failures harmed 1.5 million Americans. The cost? $77 billion. That’s not just money - it’s lost time, avoidable hospitalizations, and preventable deaths. The Caribbean has a supply chain pressure index of 8.1 - far above the safe target of -0.5. Hospitals there face weeks-long delays. Patients die waiting.





Jacob Milano on 5 January 2026, AT 01:00 AM
Man, I never thought about how my insulin could be sitting in a hot van for hours and still look fine. That’s terrifying. I’ve got a cousin with type 1 who skips doses when supplies run low - she says it’s ‘just part of the routine.’ It’s not. It’s a fucking gamble with her life.
And the fact that 78% of APIs come from two countries? That’s not globalization - that’s a hostage situation. We’re outsourcing our health to geopolitical dice rolls.
I work in logistics. We move frozen pizzas. Imagine if one wrong temperature ruined a whole batch of pizzas. We’d shut down the warehouse. But for life-saving drugs? We shrug and say ‘supply chain issues.’